https://doi.org/10.24265/liberabit.2023.v29n1.623
ARTÍCULO DE INVESTIGACIÓN
Expansion of Knowledge, Practice and Public
Policy with the ICD-11 for Psychologists and Mental Health Professionals: A Literature Review and Critical
Analysis
Luis
Hualparuca-Oliveraa,*
https://orcid.org/0000-0002-2026-3524
Estefanía Paola Betalleluz
Palominoa
https://orcid.org/0000-0001-6401-0185
aEscuela de Psicología, Universidad Continental, Huancayo, Perú
Autor corresponsal
Para citar este artículo:
Hualparuca-Olivera, L., & Betalleluz, E. P. (2023).
Expansion of Knowledge, Practice and Public Policy with the ICD-11 for Psychologists and Mental Health
Professionals: A Literature Review and
Critical Analysis. Liberabit, 29(1), e623. https://doi.org/10.24265/ liberabit.2023.v29n1.623
Abstract
Background:
Mental disorders are alterations in several functional
domains of human beings that trigger greater
morbidity and mortality if not adequately addressed. The International Classification of Diseases
11th Edition (ICD11) is a recently approved modern
global system to guide clinical
practice for these disorders and other conditions. State of the art:
Despite the imminent
implementation of this system in member states,
the guidelines on its
scientific basis, practice and importance in public health have been published
in a scattered manner, with a mainly psychiatric medical target audience, hence, it is necessary to unify these
guidelines in a single text. Therefore, the objective of this review
was to analyze three
associated aspects: (a) current knowledge of the subject, (b) its application in psychological practice,
and
(c) reflection on the implications for public health policies. To do this, these aspects
were divided into 10 sections with
the most relevant topics, and examples have been described to facilitate their use and comments to promote their understanding. Conclusions: This paper presents a review that comprehensively addresses knowledge- practice-policy triad of mental disorders
of the ICD-11.
Keywords: ICD-11; mental disorders; psychology; clinical practice; public health.
Resumen
Antecedentes: los trastornos mentales son alteraciones en varios dominios funcionales del ser humano que desencadenan mayor morbilidad y mortalidad si no se abordan adecuadamente. La clasificación internacional de enfermedades en su 11.a edición
(CIE-11) es un sistema global y moderno recientemente
aprobado para guiar la práctica clínica ante estos trastornos y otras condiciones. Estado del arte: a pesar de la inminente implementación de este sistema en los estados miembros, las guías sobre su base científica,
práctica e importancia en la salud pública se han publicado de manera dispersa, con una audiencia objetivo principalmente medica psiquiátrica; y de este hecho parte la necesidad de unificar estas guías en
un único texto. Por ello, el objetivo de esta revisión fue analizar
tres aspectos asociados: (a) el conocimiento actual del tema, (b) su aplicación en
la práctica psicológica y
(c) la reflexión sobre las implicancias en las políticas de salud pública. Para ello, estos aspectos
se han divido en 10 secciones con los tópicos más relevantes, y se han descrito ejemplos
para facilitar su uso y comentarios para promover su comprensión. Conclusiones: este artículo presenta
una revisión que aborda integralmente la triada conocimiento- práctica-política de los trastornos mentales de la CIE-11.
Palabras clave:
CIE-11; trastornos mentales;
psicología; práctica clínica; salud pública.
Mental disorders consist of significant disturbances in thinking, emotional
regulation, or behavior (World Health Organization [WHO], 2022e). Although there are effective
alternatives for the prevention and
treatment of these conditions, a large
proportion of the population does not have access to effective care. According to the WHO (2022e), one in every eight people in the
world lives with a mental disorder
by generating disability, increased morbidity and
mortality. Classifications have been designed and revised for more than a century
to guide clinical practice and
improve communication between mental
health professionals and researchers (Fiorillo
& Falkai, 2021); all this, through widely accepted descriptions of mental disorders
that allow an evaluation and
diagnosis framework for adequate intervention
of the patient (Fiorillo & Falkai,
2021; Lindmeier, 2022).
Although there are several
used classification systems
(such as the Diagnostic and
Statistical Manual of Mental
Disorders 5th edition,
text revision [DSM-
5-TR], the Hierarchical Taxonomy of
Psychopathology [HiTOP], the Research
Domain Criteria [RDoC] and the Systems
Neuroscience of Psychosis [SyNoPsis]), there is no doubt that the most important is the International
Classification of Diseases (ICD;
Columbia Psychiatry, 2022)
because of its development and global
applicability; which
not only describes
mental disorders, but also all known diseases, possible causes and determination of their manifestation
and joint influence (WHO; 2022d). The
ICD revisions have taken into account (vertical) compatibility with the entire WHO family of international classifications and mutual (horizontal)
compatibility with the United Nations
(UN) families of international classifications (Guggenheim, 2013); which together allow a
multidisciplinary and multisectoral approach to mental disorders
(Hualparuca-Olivera et al., 2022). ICD-11,
recently approved for use (WHO,
2022c), includes mental disorders in one of its chapters
called Mental, Behavioral
or Neurodevelopmental Disorders
(ICD-11 MBNDs). This chapter presents the challenges
and opportunities for health professionals, administrators, and authorities of member states
in this new era.
In this sense, the current
practice of clinical
psychologists requires an understanding of the ICD- 11 standards to be able to code properly and conduct a complete evaluation (i. e., case formulation) in order to improve mental health of their patients (Stein et al., 2020). Because the ICD-11 does
not fully describe the causality of
the diagnoses, it does not aim at
what underlines a symptom, for therapeutic purposes,
but rather at the phenomenology of each symptom
(Kountouras & Sotirgiannidou, 2022; Stein et al., 2020). For that reason, it is
possible that the assigned ICD-11
diagnosis serves as a first route to design
an evidence-based intervention specific to a
disorder, if this is unique and has a great adjustment to
the clinical manifestations of a
patient (very atypical situation);
otherwise, psychologists will have to rely on
case conceptualization strategies with a more in- depth evaluation to plan a treatment according to the individual needs of the user (The Psychology Practice, 2021). Certainly, this last route allows
clinicians to intervene in the
symptoms of a patient with relative independence
from the diagnostic categories of the ICD-11-MBNDs.
From a biopsychosociocultural
approach, mental health practice is
often based on the knowledge and integration of psychotherapeutic theories and techniques to define the complex interactions between health factors (Hooley et al., 2021). Therefore, by integrating the lifespan and stepwise
approach, and recognizing the natural course of the disorder
(Gaebel et al., 2022;
Stein et al., 2020; Vujnovic et al., 2021),
psychologists must analyze the relationship of personal history; which includes biopsychosociocultural risk and
protective factors, whether distal (past) and/or proximal (current) (Hooley et al., 2021), with clinical manifestations of the disorder
(including current behavior).
In addition, psychologists must
measure the impact of the disorder on social impairment and
assess subjective personal
experiences (e. g., distress; see Regier et al., 2020). As they do so, it is pertinent to consider the cultural characteristics
(geography and language) of patients (Sharan & Hans, 2021), establish a differential diagnosis of the disorder and an etiological diagnosis of the deterioration; and define a treatment guideline according to the needs of the patient
(Kielkiewicz, 2019). Psychologists must know
and apply
psychiatric, psychological (and
legal, if required) terminology in addition to using the standard methodologies
for research (and teaching) with the best possible
evidence to guide (and even lead) public policies
(see Saxena et al., 2012). An
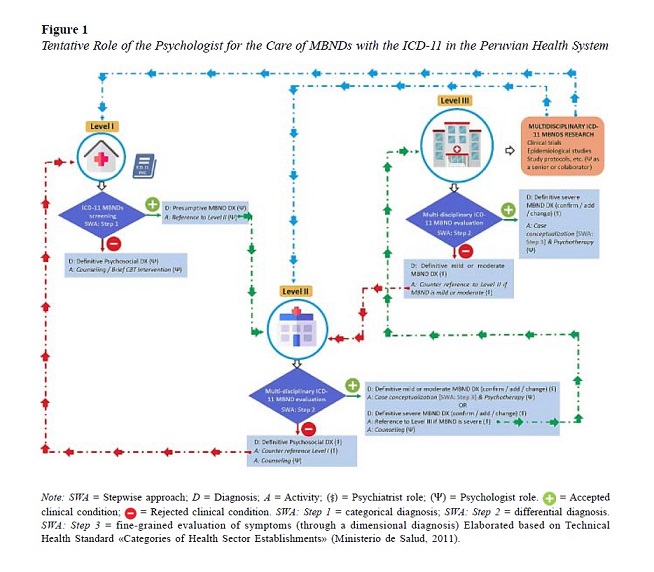
overview of the role that Peruvian
psychologists would play in caring
the MBNDs with the ICD-11
is shown in Figure 1.
Consequently, this paper offers a review to address the science-praxis-policy triad by using understandable terminology for psychologists. In addition, to reinforce collaborative work in this review for the sake of ICD-11
implementation, terminology compatible with other professions that
work closely with mental health was also used. Certainly, the practice
and public policies analyzed in this review is
focused on the Peruvian reality, but they can be adapted to other realities.
ICD is the international standard for
systematic recording, reporting, analysis, interpretation, and comparison
of mortality and morbidity data (Lindmeier & Joi, 2018; Reed, 2010). The 11th revision is the result of a collaboration between health professionals,
statisticians, epidemiologists,
encoders, translators,
experts in classification and information technology (IT) from around the world (Lindmeier & Joi,
2018). As Youmans (2022) mentions, the ICD- 11 is a scientifically rigorous product that accurately reflects contemporary health and clinical practice and represents a significant improvement on
previous revisions. In this sense, the objectives
of the implementation were
(1) to guarantee that the ICD- 11 works in an electronic
environment, (2) to provide a multipurpose classification by guaranteeing consistency and interoperability between
different uses, and (3) to provide
an international and multilingual
reference standard which allows scientific
comparability (WHO, 2022d).
The ICD-11 classification system
integrates 26 chapters, including chapter 6
about mental, behavioral, or neurodevelopmental disorders, and includes
a supplementary section for
functioning assessment, referring
to groups of diseases with more than 17 000 flexible alphanumeric codes, more than 120 000 coded entities and with the indexing of more than 1.6 million clinical terms to these coding entities (Pezzella, 2022;
Regier et al., 2020). These codes range from 1A00.00 to ZZ9Z.ZZ including a letter as the second character to differentiate from the ICD-10
(Hyeji et al., 2022). As Caux-Harry
(2018) mentions, ICD-11 changes category
codes from 3 characters (characters to the left of the decimal)
to 4, with an alphabetic character in the second
position and a number always in the third position; thus, the first character of any code symbolizes the chapter number. For
chapters 1 to 9, the first character
of the code corresponds to the chapter
number, whereas for chapters 10 to 26, the first character is a letter (Caux-Harry, 2018). Consequently,
all codes of the same chapter always start with the same character; furthermore, the number of characters in the code varies from 4 to 7 (International Federation of Health Information Management Associations [IFHIMA], 2021).
The basic
structure, characteristics and
substantial changes of ICD-11 compared
to its previous revision are better described in Hyeji et al. (2022).
The ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS) has two
online/offline systems: (a) an online browser which is an enlarged
electronic version of a tabular list
in English, Arabic, Spanish, French,
Russian, and Chinese (see Harrison et al., 2021);
(b) a coding tool that is used in a
similar way to the alphabetical
index in previous revisions, but with several
enhancements to facilitate accurate, simple, and fast coding;
(c) a reference guide describing an introduction to the context, components, and intended
use (WHO, 2022d);
and (d) a maintenance platform
–WHO-FIC Maintenance Platform–, where modifications or
additions can be proposed (IFHIMA,
2021). The ICD-11 is currently used in 35 countries
(WHO, 2022c) and several decades will possibly go by until there
is a new review (Regier et al., 2020).
The ICD-11 has a dimensional approach that allows adding specific
categories pertaining to current symptoms, severity, and course of
illnesses to better track changes over time. As mentioned by Lindmeier and Joi (2018), this classification system
contains the WHO nonproprietary names for drugs, clinical documentation,
allergology, reimbursement, primary care, causes of death, cancer registry,
patient safety, dermatology, pain documentation, and data dictionaries for the guidelines related to ICD-11. Additionally, in response to the
COVID-19 pandemic, codes have been developed
to confirm the diagnosis, categorize it as a cause of death, categorize post-disease problems, document the vaccination procedure, and identify any negative impacts on them,
among others (Harrison et al., 2021; Lindmeier & Joi, 2018).
As mentioned by Reed, Sharan, et al.
(2018), an ideal classification system ensures reliable diagnosis of mental disorders. Moreover, it can be clinically
useful and applicable worldwide
(Keeley, 2016). Thus, a proper identification of a person’s mental health needs is ensured to provide adequate and cost-effective treatment
(Reed, Sharan, et al., 2018). With this objective, a
series of studies and reviews have been carried
out by psychiatrists and psychologists when designing chapter 6 of the ICD-11: mental, behavioral, or neurodevelopmental disorders (ICD-11
MBNDs; Keeley, 2016; Keeley et al., 2016; Kulygina et al., 2021; Reed, Keeley, et al., 2018; Reed, Sharan, et al., 2018); which resulted in a preliminary product,
the ICD-11 Clinical Descriptions and Diagnostic Guidelines (ICD- 11 CDDG).
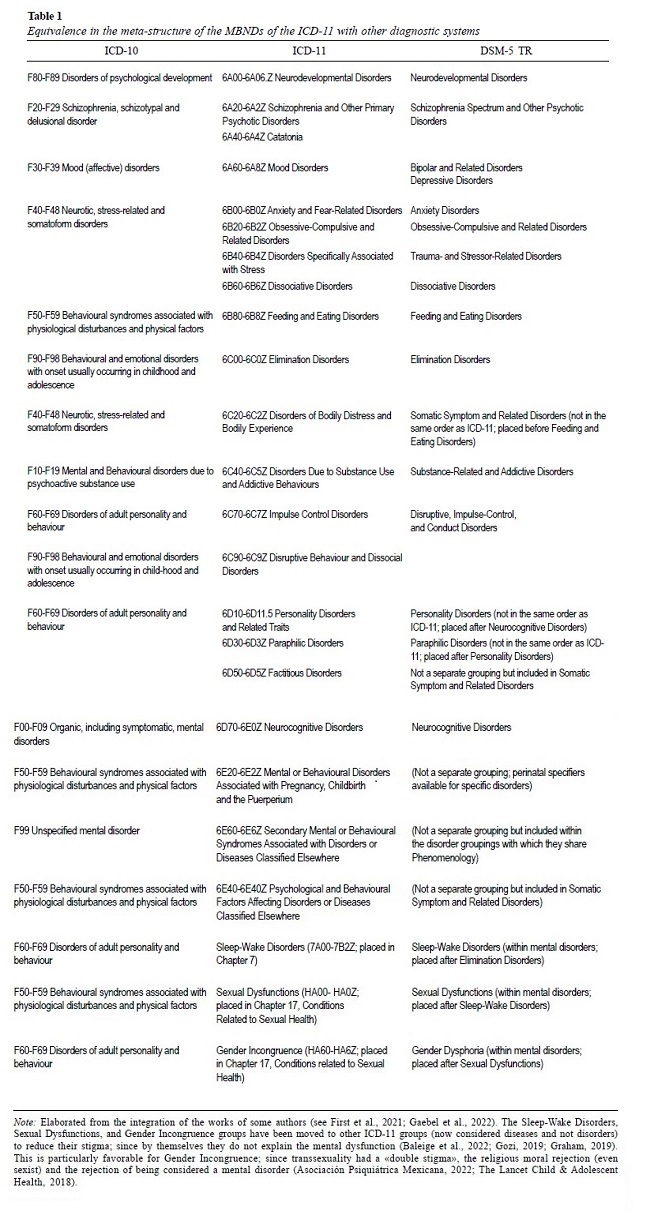
Chapter 6 of the ICD-11
contains 21 sets
of diagnostic categories for Mental, Behavioral, or Neurodevelopmental Disorders - MBNDs (see Table
1). The ICD-11 CDDG contains information about
each of the groups of diagnostic categories concerning the
ICD-11 MBNDs in addition to the statistical version of this chapter, which is displayed on their offline/online systems alongside the other medical
conditions listed above.
Owing to a worldwide partnership of healthcare
professionals, this document was created as
a project to assist in the diagnosis of the practice of mental health professionals, and it was accessible until 2021 in the global clinical
practice network (GCPN).
The goals of the ICD-11 related to CDDG
were to: (a) collect data and information systematically; (b) use a longitudinal approach rather than a
transversal conceptualization; and (c) concentrate on more practical indices such as comorbidity and
long-term disability (Vujnovic et al., 2021). The
final product of this project, also published in the GCPN, replaced the ICD-11 CDDG and was called the ICD-11 Clinical Descriptions and Diagnostic
Requirements (ICD-11 CDDR). The
ICD-11 CDDR contains, in addition
to the aforementioned diagnostic guidelines, considerations related to the limit of normality
(threshold), characteristics of the course, development,
culture, sex and/or gender, and the
limits with other disorders and conditions (differential diagnosis). The ICD-11 CDDR is not part of a separate
section or book but is implemented in the ICD-11
for MMS itself as part of the structure of its
diagnostic categories.
For centuries,
mental disorder classification
systems have focused more on inter-rater reliability than on the
clinical usefulness of diagnostic categories, resulting in clinicians who do not easily
understand or apply diagnoses, which
makes it difficult to identify and adequately
treat people with mental disorders (Keeley, 2016). In the ICD-11 MBNDs chapter, an attempt was made to simplify this situation by eliminating or merging categories that were not useful, and flexible guidelines were established to improve their cross-cultural
applicability (Keeley, 2016). The
structural changes in this chapter were primarily:
(a) the elimination of disorders of
sleep and wakefulness and disorders related
to sexual health, currently grouped into two
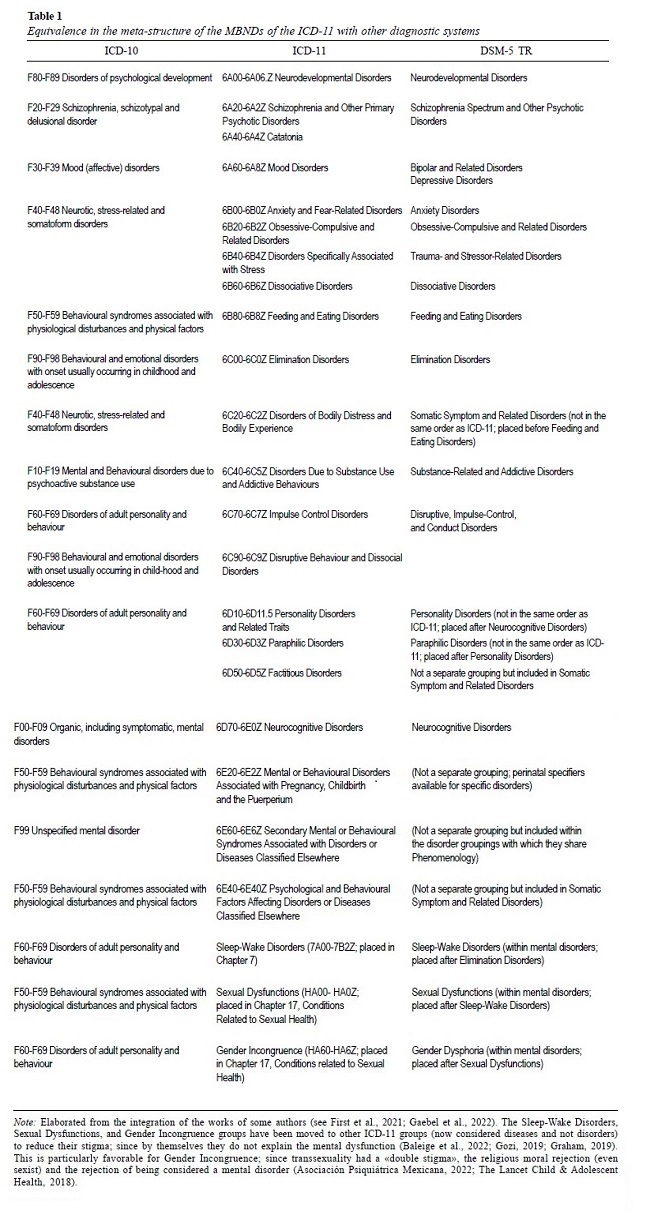
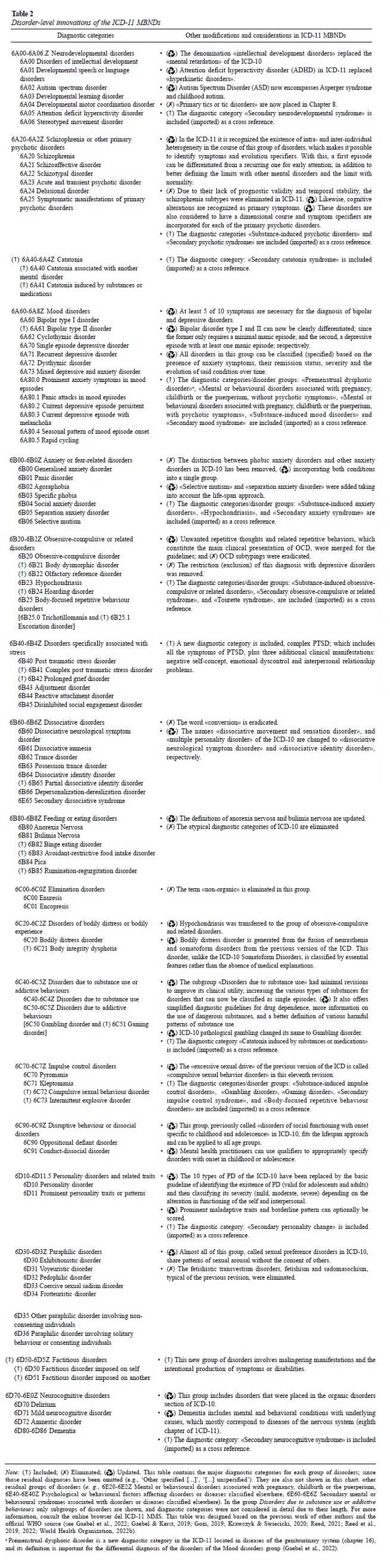
separate chapters recently integrated (Gozi, 2019); and (b) the addition of various new diagnoses (see Gaebel et al., 2022).
These new mental
disorders were added
to (i) optimize the usefulness of morbidity statistics; (ii) facilitate the identification of clinically important
but misclassified mental disorders
to provide appropriate management; and (iii) promote the investigation of more effective treatments (Reed et al.,
2022). For more information on the amendments at the disorder
level, see Table 2.
Other
additional changes correspond to the dimensional
perspective that is implemented
within the diagnostic categories because the evidence
has shown that MBNDs
represent, for the most part, the interaction of latent dimensions (Columbia Psychiatry, 2022;
Reed, 2021; Roessner et al., 2016). This dimensional perspective promotes a recuperative approach to the care of these conditions
instead of treating them as chronic (Regier et al., 2020), labeling and generating stigma towards patients (Asociación Psiquiátrica Mexicana, 2022). Likewise, it offers the opportunity
to intervene in specific problems with specific
interventions, according to the complexity level
(comorbidity) of the cases, thus also defining
health care needs (Reed, 2021).
Evidence has shown that: (a) the clinical
manifestations of adult disorders occur similarly in childhood; (b) child and adult disorders appear to be continuous,
as many young adults with psychiatric disorders (neurodevelopmental, emotional, and behavioral) have had psychiatric diagnoses
in adolescence (Garralda, 2021); –e. g., separation anxiety disorder or avoidant/restrictive food intake disorder are diagnosable in both children and adults–. Based on this evidence
and in line with the taxonomy proposed in the DSM-5, the ICD-11 working group
made the decision
to modify the location of childhood mental
disorders and merge them into ICD-11 categories. Thus, all diagnoses
offer a lifespan approach (i. e., with a longitudinal focus on human development) and an explicit set of instructions about the ways in which manifestations vary by age (Garralda, 2016).
The ICD-11 MBNDs category groups
–unlike the Kraepelinian organizational structure (Gozi, 2019)– begin with diagnoses that reflect disturbances manifesting early in life development (Garralda, 2016); e. g., 6A00-6A06.Z neurodevelopmental disorders,
and 6A20-6A2Z schizophrenia and other primary
psychotic disorders, followed by diagnoses that
manifest more frequently in adolescence and early adulthood,
such as 6A60-6A8Z mood disorders, 6B00-6B0Z anxiety and fear-related
disorders; and diagnoses relevant to
adulthood and later life, such as 6D70-6E0Z neurocognitive disorders (Gozi, 2019; Regier et al.,
2020). Within this overall framework, each
disorder now aims to describe variations in children’s
presentations, and children’s most typical diagnostic
categories are those appearing in the first
years of life, neurodevelopmental disorders, disruptive behavior, and dissocial disorders (Garralda, 2016).
Neurodevelopmental disorders
mainly include: 6A00 disorders of intellectual
development, 6A01 developmental speech or language
disorders (including alterations related to language
and speech sound/fluency), 6A02 autism spectrum disorder, 6A03 developmental
learning disorder, 6A04 developmental motor coordination disorder, 6A05
attention deficit hyperactivity
disorder, 6A06 stereotyped movement disorder,
and other residual diagnostic categories. These
disorders, which may be comorbid, have an early
onset in a person’s life with the potential to
induce lifelong impairments (Roessner et al.,
2016). In addition, their symptoms
are characterized by delays,
excesses, or deviations in the fulfillment of the maturation achievements of normal
development. Autism spectrum
disorders (ASD), –which include autism, Asperger
syndrome, and disintegrative and generalized developmental disorders–, comprise a dyad of alterations in social communication and restricted repetitive behaviors (Garralda, 2016).
It is recognized in ICD-11 that
individuals with ASD frequently exhibit
simultaneous degenerations in language
and intellectual function, which probably generate the loss of some skills
(previously acquired) without
the presence of a neurological disorder (Garralda, 2021). These limitations should be considered
for the scope of multidisciplinary support, treatment planning, and selection
of effective individualized interventions. Likewise, specific language disorders cause significant limitations in the ability to communicate and can also be
classified based on the main focus of
the alteration, either in receptive language
or in expressive (pragmatic) language. A possible guideline for the
differential diagnosis of specific
language disorders and ASDs is the
lack of repetitive and restricted interests that characterize the latter (Garralda, 2016).
On the other hand, disruptive behavior and dissocial disorders mainly include 6C90 oppositional defiant disorder (with qualifier/subtype: with and without chronic irritability-anger), and 6C91 conduct- dissocial disorder (with qualifier/subtypes: childhood onset and adolescence; and it is the
earliest onset with a poorer prognosis). Both disorders have a qualifier with limited prosocial emotions
in children who are identifiable, relatively stable, and linked
to a more severe, aggressive, and stable pattern
of antisocial behavior.
Intermittent explosive disorder, kleptomania, and pyromania may be classified in this section if they are chronic; or in a
separate group of impulsive
disorders, if they are episodic (Garralda, 2021).
To date, findings from field studies
conducted in children and
adolescents have confirmed adequate levels
of validity and reliability of the CDDR for diagnosing
oppositional defiant disorder, attention deficit hyperactivity
disorder (ADHD), mood disorders,
anxiety, and fear-related disorders, reinforcing its global
applicability (see e. g., Robles et al., 2021).
The differences between the ICD-11 and
DSM- 5-TR (American Psychiatric
Association, 2022) are intentional because they are directed toward different goals.
This is because
the former is the product
of the collaborative work (non-profit) of experts from different professions (in addition to authorities) from 159 member states; while the latter configures a (commercial) franchise of the work of experts from a single
profession and from a single country (Asociación Psiquiátrica
Mexicana, 2022; Columbia Psychiatry, 2022). The DSM-5-TR has a more research-oriented (and less practice-oriented) approach
because it has rigid diagnostic criteria (e. g., criteria A, B, etc.), which are expected to maximize the
reliability of diagnostics in
different environments (Appelbaum, 2017; Bach et al., 2022; Stein et al., 2020). In contrast,
the MBNDs of the ICD-11 have a more pragmatic approach because they incorporate flexible diagnostic
guidelines (vignettes), considering in a deeper way the variability of diverse cultures and
limitations of the different levels
of health care, –even in low-resource settings– (Appelbaum, 2017; Bach et al., 2022; Stein
et al., 2020).
The chapter groups of the ICD-11 MBNDs
are listed in Table 1, which also
includes a comparison with the DSM-5-TR meta-structure; –for further details on the differences and similarities in diagnosis between ICD-11 MBNDs and DSM-5-TR
consult First et al. (2021) and
O’Brien (2022)–. In general, the comparability
of the structure of the two classifications
can be considered a success of the harmonization
efforts between the WHO and APA. Some structural
differences reflect ICD-wide conventions related to residual categories and mental disorders associated with other underlying illnesses.
The discussions in
which the WHO, the Advisory Group, and the various
Working Groups took part resulted in other differences, such as those regarding the diagnosis and treatment of children
with chronic irritability and anger,
compulsive sexual behavior disorder, personality disorders, substance use/ substance
dependence, and somatoform disorders. Another
distinction is that the new chapters of the ICD-11 include the classification of «organic» and
«non-organic» components of sleep-wake disorders, problems relating to sexual health, and gender identity in ways that are connected with the most
recent research and clinical
practice (O’Brien, 2022).
Regier et al. (2020) stated that one of the similarities between the two diagnostic systems is the incorporation of a dimensional approach
for some disorders within their categorical system. The debate
between the psychoanalyst’s
approach to the dimensionality
of mental disorders, and the discrete categorization of these conditions from the neo- Kraepelinian approach, can lead to a better understanding of the disorders through the
description of the etiological factors,
characteristics, and clinical
course of the disease, supplemented with symptom scores. Accordingly, for some ICD-11 and DSM5- TR diagnoses, dimensional expansions regarding severity,
course, and specific
symptoms were added.
Some examples of ICD-11 include autism spectrum disorders (ASD), personality
disorder, depressive or bipolar
disorders, and primary psychotic disorders (Alves et al., 2020; Gaebel et al., 2022); while in the DSM-5 TR, they are autism spectrum
disorders (ASD), attention deficit/hyperactivity disorder, bipolar
disorder, and major depressive disorder (Regier et al., 2020).
According to Michael B. First, co-chair and editor of DSM-5-TR, the differences
between ICD-11 and DSM-5 TR provide four main advantages and disadvantages (as cited in O’Brien, 2022): (a) it enables classifications to be improved
to satisfy user group
needs; (b) it also supports growing clinical
research validity over time; (c) it encourages frequent evaluation of the best nosological approaches; (d) finally, opportunities were created for those working
on the development of diagnostic and measuring tools. However,
these variations are disadvantageous because:
(ii) they make it more difficult to gather and report health statistics in countries that use the DSM;
(ii) they make it more difficult to compare the findings
of studies that were assessed using various systems;
(iii) they make it more difficult to evaluate
and approve drugs for patients
whose medical indications were prescribed using various
systems; and (iv) they add to the
workload for those who create
diagnostic tools and measurements (O’Brien,
2022).
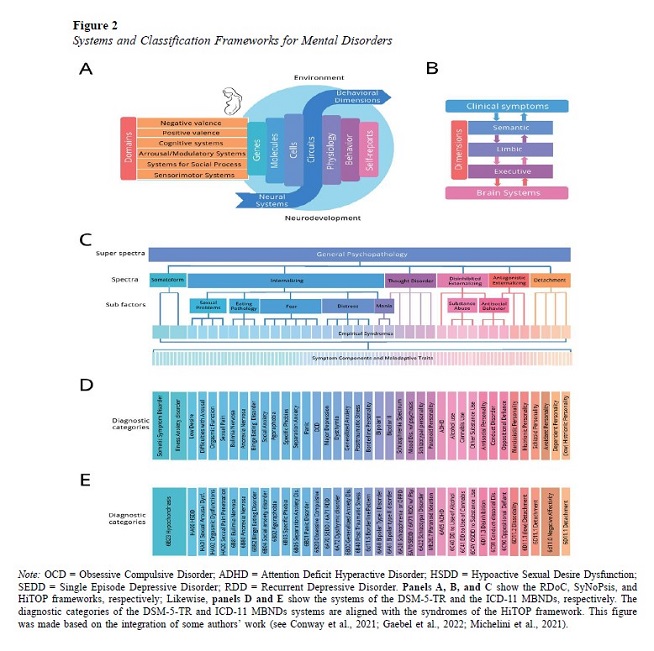
In recent years, three approaches have been introduced
in psychiatric nosology: HiTOP, RDoC and SyNoPsis –see Figure 2 for more detail on the constructs of these approaches–. As Gaebel et al. (2022)
mentioned, these frameworks were developed from a dimensional perspective to enable more accurate and nuanced knowledge of mental
disorder assessment and diagnosis
of mental conditions, rather than categorical descriptions that
reduce the validity and reliability of mental disorders
(Strik et al., 2017). The first of them (HiTOP),
designed by the HiTOP Consortium, seeks a classification based on the multivariate phenotype of clinical conditions; and the remaining two, –RDoC from the National
Institute of Mental Health in the USA (NIMH) and SynoPsis from the Bern University
Hospital of Psychiatry
in Switzerland– an etiological explanation based on the neurobiology and pathophysiology of these conditions.
Currently, these three frameworks have
deficits in terms of their global and clinical applicability (utility) because
they are: complex
for practice and culturally variable (Gaebel et al., 2022; Sharan & Keeley, 2018), –mainly in the case of HiTOP–; and practically
inaccessible and do not have convincing evidence of the neurobiology-psychopathology association (Gaebel et al., 2022;
Regier et al., 2020),
–mainly in case of RDoC and SynoPsis–. In the future, if science
demonstrates a harmonization of the RDoC or
Synopsis units of analysis with syndromic manifestations, these neurobiological frameworks may be incorporated into future versions
of the ICD; –only if they have evidence
of acceptable diagnostic validity and are practical in
routine settings (Gaebel et al., 2022)–. Gaebel et al. (2022) mention that HiTOP can be incorporated, but only in
specialized mental health units; however,
given its complexity, it will
not be able to offer substantial changes in the classification of these systems. Recent preliminary evidence
has rejected HiTOP as complex to use (see
Balling et al., 2023); however, more study is still needed
on this subject.
As mentioned by some authors,
a potential problem
with current categorical classification systems is that they were designed
for global applicability in
various settings, which could lead to the
loss of construct validity (Gaebel et al., 2022; Maercker, 2022). Complex frameworks such as RDoC or HiTOP are suitable for research purposes, while the categorical classification system
in ICD-11 provides greater clinical utility (Gaebel et al., 2022; Regier et al., 2020). For this reason, researchers often prefer
detailed dimensional assessments; while primary care mental health professionals need diagnostic categories that are easy to understand and communicate (e. g., referrals and counter-referrals) (Gaebel et al., 2022). However,
the strengths of these dimensional frameworks can already be
used by the member states,
including Peru.
Gaebel et al. (2022) emphasized that to ensure that future versions of the ICD meet the needs of different user groups, it is pertinent that a gradual procedure for diagnosis (i. e., a stepwise approach) be implemented. In this approach, each diagnostic step
describes the patient’s psychopathology in greater detail.
In step 1 of
the diagnosis, a patient’s symptoms
can be classified into broad
diagnostic categories, as suggested in the primary care version of ICD-11, –e. g.,
for the identification and management of mental disorders in the first level of care of Peruvian health establishments (levels of care from I-1 to I-4 of the establishments
of the Ministry of Health [MINSA])–. In this step, patients suffering from a degree of distress who require additional
diagnostics and specialized
interventions can be
identified. In step 2, a more
specific differential diagnosis can be made. The ICD-11
CDDR provides detailed
descriptions of the core symptoms of
disorders, boundaries
with normality, and guidelines for differential diagnosis. This step can be performed in
the second and third level of care (e. g., from II-1 to III-E of MINSA establishments). Once the disorder
has been identified and differentiated, reassurance, brief cognitive interventions can be performed for a
mild level of disorder severity.
Step 3 of the diagnosis enriches
categorical diagnoses with
dimensional assessments in research settings
and specialized interventions to pin down psychopathology; –e. g.,
also at the second and third level
of care (specialized care)–. Thus, the advantages of both approaches can be combined (e. g., for the diagnosis of schizophrenia or other primary psychotic disorders). Specifically, the result of each categorical diagnosis can be
complemented with a symptom profile
that provides specific
information about the domains involved. In this step, users with moderate and severe personality disorder can be cared for. In
moderate cases, brief cognitive
interventions, less intensive structured psychotherapies are used; whereas,
in severe cases structured
intense psychotherapies and medications are used (Mulder,
2012). Similarly, counter-referrals can be issued if mild or
subclinical levels of the disorder
are found. Bach and Simonsen (2021) mentioned
that the disorder severity configures a decision tool for clinical management and the intensity of required treatment (involving the need to establish epistemic trust, level of support approach and strength of the therapeutic alliance).
Consequently, with the stepwise approach, prompt communication based on diagnostic categories is promoted; and dimensional assessments will provide more nuanced profiles for contexts where
detailed dimensional information beyond the overall degree of severity is needed to inform treatment (e. g.,
psychotherapy) and research. The stepwise approach covers only some groups of disorders in
ICD-11. However, there is great
potential for enriching more categorical diagnoses
with dimensional symptom
profiles. For example, experts have recommended assessing all symptoms
of substance use disorders in the DSM-5-TR
on (at least) a 3-point
scale; initiative which can be implemented in later
versions of the ICD (Gaebel et al., 2022).
One should consider (a) genetic abnormalities, (b) brain
dysfunction and neuronal plasticity, (c)
hormonal and neurological
abnormalities, (d) neurotransmitters in the brain or other parts
of the central nervous system, and (e) temperament when examining biologically
based abnormalities for potential
diagnosis of any MBND ICD-11 (see Hooley et al., 2021). The ways
in which the environment can
influence the genotype (genotype-environment correlations), the ways in which the genotype can
influence the phenotype, and the ways in which genetic vulnerabilities can
influence the development of mental disorders (environment-genotype interactions) are some of the proposed
objectives in the biological
investigation of MBNDs (Hooley et al., 2021; Kring
& Johnson, 2021). Adoption, twin,
and family history studies are all ways to examine how much genetic and environmental factors
play a role. However, recent research has concentrated on employing
linkage analysis and association studies to identify the precise position of genes that contribute to mental diseases
(Hooley et al., 2021).
According to Hooley et al. (2021), the
results of these studies showed that
there are 1000 (distinct) genes that influence with a certain degree of vulnerability
(diathesis) to schizophrenia; and some of
these genes are also found in severe depressive disorder, 6A02 autism
spectrum disorder (ASD), bipolar disorder and in 6A05 attention
deficit hyperactivity disorder
(ADHD). On the other hand, studies of
neuronal plasticity have shown that
the genetic makeup of brain development is not fixed
as existing neural circuitry can be often modified based on experience. Additionally, various neurotransmitters
(primarily serotonin, dopamine, norepinephrine, glutamate, and gamma aminobutyric acid) and hormonal abnormalities (primarily the hypothalamic-pituitary-adrenal, axis with
activation of corticotrophin,
adrenocorticotropic, epinephrine [adrenaline], and cortisol) contribute to the development of different mental disorders
because of their effects on specific
areas of the brain and body.
Likewise, temperament –strongly
influenced by genetics– configures the set of characteristics for reactions and self-regulation to
environmental stimuli. Temperament
also constitutes the basis of adult personality and influences vulnerability to various disorders
(Hooley et al., 2021).
Psychologists must consider these
vulnerabilities mainly at the time
of case conceptualization, and treatment
planning. To control the associated acute symptoms of these vulnerabilities, immediate psychiatric care is crucial –e. g., the above- mentioned
schizophrenia or ADHD, which are more strongly associated with alterations in biological domains
as established by the organization of ICD-
11 MBNDs through the lifetime approach–.
Additionally, in specialty care health centers (e. g., hospitals), patients with life-threatening, degenerative, and/or chronic medical
conditions (e. g., 2C61 Invasive
breast carcinoma) may develop psychiatric conditions (e. g., 6E62.2 Secondary mood syndrome, with mixed symptoms). In these circumstances, multidisciplinary and coordinated work between doctors, nurses, psychologists, and
clinical social workers is needed to achieve adequate
knowledge of the disease and develop coping strategy and adherence
to psychological and medical treatment (Semple & Smyth, 2019).
The ICD-11 stems from the medical model, where the disorder is identified solely through its symptoms, and the typical treatment is to eliminate them through medication, without the need
to identify and treat its causes. If
only this approach is used, mainly for severe
levels of the disorder, it is possible that the patient develops dependence on the medication and the symptoms reappear
once it is discontinued (Kielkiewicz,
2019). For example, a meta-analysis showed
that a combination of psychotherapy and pharmacotherapy produces
more effective outcomes
against major depressive disorder than each of these treatments applied individually (i. e., monotherapy; Kamenov et al., 2017). Although there is some interpretation bias, another umbrella
review also demonstrated the superiority of combined
treatment in cases of ADHD, complex
post-traumatic stress disorder (PTSD)
and Social Anxiety compared to monotherapy (Leichsenring et al., 2022).
Given this, the psychological interpretation of the patient’s
condition, through psychological theories, is important for the psychotherapeutic approach (Peterson, 2009).
Certainly, science cannot find
replicability of the results to
identify genetic and environmental agents, or
their degree of influence in the development of a mental condition; consequently, these cannot be generalized. However,
based on the individual psychological evaluation,
conceptualization of the case, psychodynamic definition of the problem, functional analysis and other strategies
used by the psychologist, it is possible
to find the causal components
(or at least the most influential central components
in the deterioration) for the development, maintenance, and exacerbation of other symptoms
or signs of the disorder(s)
(Kielkiewicz,
2019). Intervening in these causal agents from the individual intervention, and progressively with group therapies, pharmacological treatment can be enhanced,
and eventually discontinued without fear of relapse.
A psychologist, unlike a psychiatrist –as is traditional– must delve deeper into the patient’s
problem. Psychiatrists often have a high demand for patients (often
continuators) and therefore, reduce
their attention
time (Evans et al., 2013; Guggenheim, 2013); which probably also affects rapport (Patel et al., 2017). Additionally, patients may feel less
stigmatized and better understood in
a psychological consultation because
psychologists, unlike psychiatrists, assign fewer diagnostic categories to a patient (Evans
et al., 2013). According to Evans et al. (2013), these different perspectives on the patient’s mental
condition lie in main issues such as: theoretical perspectives, training, professional
activities, the services provided,
the served patient populations,
and health policies. The stigma must
certainly be of particular interest and care for psychologists to address and reduce its effects on patient
care.
Although both types of mental health practitioners are responsible for treating patients with compassion, empathy,
and dignity, psychological care produces more
relief than psychiatric consultation because of the emotional and therapeutic link that is created. Moreover,
in psychological care, people are not usually labeled as «depressed» or «schizophrenic», and active listening and other interview
techniques based on emotional reflection are used. Also, a feedback based on psychological theories
is carried out to obtain an understandable, assertive, and compassionate message
of the psychiatric condition.
Psychologists are aware of two fundamental problems: (a) Psychiatric diseases are severe forms of internal experience and behavior, due
to sadness, rage, and anxiety; which are common human emotions; (b) unlike other medical conditions (illnesses),
mental disorders generate more prejudiced and derogatory assumptions than other types of medical conditions (Miles, 2018). The
patient is not to blame for having
a disorder (Corrigan et al., 2014), and probably does not deserve to be
objectified with these adjectives.
Considering the role of the psychologist
for the management of diagnostic
categories of the ICD- MBNDs (see Figure 1), prevention would mainly lie in the adequate detection (presumptive
diagnosis) of the MBNDs, their subclinical levels and the psychosocial
factors present that affect the patient; this
is followed by a brief CBT approach or referral as appropriate. For this, the psychologist and health professionals at the first level of care
must receive training for proper management
of step 1 of the stepwise approach
(categorical diagnosis) using the ICD-11-PHC and ICD-11 MMS as a guide.
At the second level of care where confirmation of the clinical condition is required in
a precise and refined manner (steps 2 and 3 of the stepwise approach), the psychiatrist must assign the definitive diagnosis of the ICD-11 MBNDs
after a multidisciplinary evaluation
with the psychologist and/ or a nursing professional specialized in mental health
issues. This diagnosis must be complemented with a case formulation that includes the anamnesis, current
behavior, presentation of symptoms, subjective experience of the user and social functioning. After that, the psychologist will be able to establish the most appropriate therapeutic regimen for the
case (see e. g., Kramer, Eubanks, et al., 2022); being able to predict
the estimated time of therapy,
possible complications –e. g., abandonment of therapy, usual in patients with 6D11.5 Borderline pattern
(Arntz et al.,
2022; Iliakis et al., 2021); or refusal of therapy, typical
in patients with 6D11.2 dissociality in personality disorder or personality difficulty (Herpertz et al., 2022)–, possible acute
episodes and comorbidities with other conditions and/or mortality outcomes. These predictions will also provide
psychologists with possible
treatment/approach alternatives to initiate a change in the proposed
therapeutic scheme and improve the therapeutic alliance
(Kramer, Ranjbar, et al., 2022).
Likewise, the forecast extracted from
the case conceptualization will serve to establish distance
between the dates of home visits, or phone call tracking of the users. For example,
continuous (weekly)
tracking is preferable in patients with severe levels of a condition and suicidal intent –e. g., in cases
of patients with 6A71.4 recurrent
depressive disorder, current episode severe, with psychotic
symptoms / 6B41 Complex post-traumatic stress
disorder / 6D11.5 Borderline pattern
(Gelezelyte
et al., 2022)–, than in patients with mild levels or with psychosocial problems derived from judicial instances. Finally, in the third level of care where the rehabilitation of patients with severe and chronic conditions prevails, the psychologist repeats clinical management of the second level of care and accompanies and guides scientific
practice of the ICD-11 MBNDs. To do
this, it involves a multidisciplinary team in regional and national studies at all levels of care, designs and
evaluates the health care programs
and protocols of the MBNDs taking the ICD-11 as a framework and a comprehensive
and inclusive perspective.
Traditionally, the
psychological approach involves different frameworks to
treat clinical manifestations of a
disorder. For example, from the ICD-11 model,
for a patient with 6C40.2 alcohol dependence, a psychologist using
the psychodynamic framework may
interpret the condition as her attempt to reduce intrapsychic conflict and anxiety through repeated alcohol
use; and that the person when making catharsis and realizing this dynamic can find a corrective
emotional experience. On the other hand, from the behavioral framework, the same professional can interpret the disorder as the patient
learning inadequate habits to
reduce social stress; and the approach
to it is precisely aimed at modifying this learning
through conditioning factors (Hooley et al.,
2021).
As Hooley et al. (2021) stated, from the cognitive- behavioral framework, the
same psychologist can interpret said psychopathology as the irrational thought that the patient
has about his excessive alcohol
consumption as a way to reduce social
stress; and his
approach is based upon guidelines to
modify these irrational thoughts.
Likewise, from a humanistic framework, the psychologist interprets the exaggerated consumption of alcohol
as a blockage or distortion of the natural
growth of the individual
person. In
addition, the psychiatric condition can be overshadowed if the «client» promotes his virtues and achieves
self-realization. Finally, from the existentialist framework, alcohol dependence is
interpreted as a failure for the constructive management of the
«client» in the face of despair and frustration, of his own existence; and that the disorder can be dealt
with by promoting its values,
but also by managing the adverse obstacles
it may encounter.
Evidence-based psychological
interventions for specific diagnostic categories are known to be effective,
but only if they perfectly fit the patient’s
clinical manifestations; situations that are more pragmatic
but unfortunately not very common in clinical
practice (The Psychology Practice, 2021). Thus,
current practice of psychologists, at least in
specialized care, requires
comprehensive management of various psychotherapeutic techniques that have shown evidence for addressing specific symptomatic domains (Livesley, 2018; Tyrer & Mulder, 2022).
This ensures personalized therapeutic attention to individual needs
of the user. This, in turn, generates
greater efficiency within a shorter
intervention time (Tyrer & Mulder, 2022). On the other hand, in primary care where
anxious and depressive disorders
predominate (i. e., with symptoms
that represent common alterations in the somatic and emotional domains),
the progressive approach
with the behavioral
and cognitive- behavioral
approach is more effective and practical. However, for more complex
cases, –such as the
chronic emptiness presented
by a patient with a borderline pattern,
in which alterations in the volitional domain predominate–, it will be necessary to integrate these approaches with others such as the psychodynamic, humanistic, or
existential ones, according to the needs of the patient.
With this, the complexity of multiple domains can be better addressed, which
in ordered sequence are biological, somatic,
emotional, behavioral, cognitive
and volitional ones involved in the patient’s disorders. Certainly, in the domains
closest to biological components, it is simpler to assign a diagnosis and a brief and effective pharmacological and psychological
approach (cure/treatment). However, as
the complexity of the condition progresses owing to the influence
of social and cultural factors,
a complex, comprehensive, and multidisciplinary approach is necessary. In fact, this
perspective of sequential diagnosis
and intervention has been considered for the organization of ICD-11
MBNDs through the lifetime approach;
which, similar to human
development, clearly represents how clinical
manifestations deviate dimensionally (quantitatively) from normality; and they become more
complex as human subjectivity increases with personal experience. From this perspective, the
evaluation and diagnosis with the
ICD-11 must be constant since most
mental disorders by themselves are not chronic;
and they depend a lot on inadequate social functioning
strategies that make the condition last over time, creating and maintaining disability.
(a) Early deprivation or trauma
Since women frequently exhibit more internalizing disorders and males more externalizing and thinking disorders, gender also plays a
significant effect in how mental
problems appear (see Figure 2, for an adequate
identification of these disorders and their equivalence
in the ICD-11). Even though the ICD- 11 does not code gender as a risk factor, it should be considered because it helps identify the diagnosis. For example, a large part of Peruvian women
evidences a higher
suicidal risk (i. e., symptom of 6A70.3 Single episode
depressive disorder, severe, without
psychotic symptoms) and a
large part of the country’s males have a tendency towards aggression (i. e.,
characteristic of 6D11.2 dissociality in
personality disorder or personality difficulty) (Instituto Nacional de Salud Mental, 2019). With this evidence, it could be more certain
to assign a diagnosis of severe depression to Peruvian women and a diagnosis of PD
with prominent
externalizing characteristics to men in the country.
The rejection of immigrants by members
of the new culture of the current
region or nation in which they dwell is known as acculturation, a term frequently employed in the field of mental
health. This social risk factor is
codified in the ICD-11 as QE04 target
of perceived adverse discrimination or persecution. For example, in secular societies
or states, marginalized groups –such as immigrants (WHO, 2021), the gay community (File &
Marlay, 2022), the
Peruvian Andean rural community (Hualparuca-Olivera, 2022; Instituto Nacional
de Salud
Mental, 2019)– can show a greater degree of anxiety and depression due to constant
violence (rejection) they experience.
In addition, it is common to observe
cases in which legal procedures
produce distress, and if such an association is detected, the psychologist can code the current problem as QE40 problem associated with conviction in civil or criminal
proceedings without imprisonment. Often in primary and specialized care,
a Peruvian psychologist is in charge of reporting judicial cases and acts of violence in MINSA records. This serves as epidemiological support
to make decisions on budget management for infrastructure and human resources in the fight against violence and the promotion of a culture of peace. If
these cases are not registered, it is possible
that efforts and investments
would be allocated to other activities in the executive
agenda of the governments.
Although some authors refer that those
adverse factors experienced during infancy and early childhood, including those related
to primary caregivers, are the ones that have the greatest influence on
the onset of a mental disorder, the
truth is that the accumulation (quantity) of social risk factors, more than what they are, contribute to the appearance of mental conditions. Psychologists may decide if a patient’s
diagnosed disorder is accompanied by some social
risk factor or diagnose
only one or more symptoms (e. g.,
MB26.A
suicidal ideation and/or QC4B
personal history of self- harm) rather than diagnosis of a more complex entity
(e. g., 6A71.1 recurrent
depressive disorder, current episode moderate,
without psychotic symptoms)
accompanied by social risk factors
(e. g., QE51 problem associated with interactions with
spouse or partner) if the current
problem is better
explained by social
circumstances, rather than a psychiatric disorder.
In the same way, it is important to
mention that the approach to social risk factors requires multidisciplinary and intersectoral work, the generation
of government regulations and
investments, health promotion
at different levels of care, and the prevention
in primary care. A collaborative work structure is needed between
authorities, health technicians and professionals, educators, among others, to reduce these risk factors.
The way in which a social group experiences each of
the adverse biopsychosocial factors in a certain culture of a region also influences the manifestation of psychopathology (Gureje et al., 2020). The ICD-11 MBNDs working
groups have collected information on cultural variants in order to: (a)
identify cultural concepts of
distress syndrome (causes/explanations, idioms) in various
cultural groups, (b) assess the impact of culture on the manifestation of disorders and their dynamics, (c) identify the differences in the prevalence of various disorders considering the
dynamics and cultural factors
(Sharan & Hans, 2021). The result is mainly
reflected for some of the ICD-11 MBNDs. For example,
6B83 avoidant-restrictive food intake
disorder is diagnosed
mostly in populations of low and middle- income countries (LMICs)
who avoid food intake for fear of generating somatization (Sharan & Hans, 2021; Sharan & Keeley, 2018). Likewise, category 6B04 social
anxiety disorder has a marked
cultural variant in Asian countries (e. g., Japan and South Korea) as
fear of offending others; more than the fear of being evaluated (offended or mocked) socially
(Sharan & Hans, 2021).
An applied example of this variability
in Peru is found in the distress
symptoms of 6B43 Adjustment disorder;
which in Quechua-speaking communities is referred
to as «sunquymi llakisqa kachkan» which can
be translated as «my heart is sad» since the
patient attributes to a part of her body –in this case, her heart– feeling
worried about an adverse situation and not knowing
what to do, which generates
impotence and sadness (Paniagua, 2018; Sharan & Hans, 2021). Spanish-speaking patients, who are native Quechua
speakers, frequently use the term «mi cuerpo hizo razz» to describe
somatic anxiety –as a
Peruvian expression of «ataque de nervios»
(see Paniagua, 2018) in 6B01 panic disorder–
in the form of muscle
contractions that cause the skin to stand on end. Another common attribution in these Spanish- speaking
Peruvian Andean communities (with Quechua
as their mother tongue), –specifically in relatives who attend consultation together with the patient having psychotic symptoms–, is the phrase «su cabeza está débil»
since they think that hearing voices is a product of undernutrition, and consequently
the weakness manifests itself in their head
(as an Andean folkloric explanation of this condition; Quiroz-Valdivia et al., 1997).
In the same way, habits and behaviors
that may appear to be signs of detachment
traits of a personality
disorder (PD) are common behavior in remote
communities of Andean areas whose main economic
activity is mining. In these places, where intense cold is experienced, and with an institutionalized mining economy, –which means that social contact is scarce–, normal behavior can appear to be perceived as a sign of mental
alteration if the psychologist who evaluates them is a foreigner (Hualparuca-Olivera,
2022). Moreover, it is common
for patients to attribute the cause of a mental disorder to witchcraft. This cultural group
certainly does not have sufficient
terms to report a mental disorder and often refers to external
entities to confirm
its possible cause. This leads this community to seek
the service of sorcerers and healers
who recommend them to perform
mystical rituals
instead of seeking
help from mental
health professionals.
Other disorders, in which there is cultural variability in the prevalence and subjective experience of certain symptoms, more than others, are those manifested in: depression,
adjustment disorder. Unlike its previous version
and the DSM-5-TR, in the ICD-11 CDDR it has been decided to eliminate culture-specific diagnostic categories, and sections have been created
to explain possible cultural variations for each disorder (Sharan & Hans, 2021). This change
still generates debate both for the
practice and for the research of the
ICD-11 MBNDs, which mainly argues for two opposing
reasons: (a) the designation of vignettes, instead
of criteria, facilitates the cultural adaptation of diagnostic categories in clinical
practice (Bach et al., 2022); b) the designation of vignettes reflects the lack of interest from the WHO in compiling
exhaustive information on culture
as the priority of scientists is to
find biological markers (Seligman, 2019),
rather than cultural markers in their desire to
universalize the diagnostic system (Sharan & Hans, 2021).
Although the first statement has been continually supported by the ICD-11 MBNDs working group in its research, it is also true that most
of this has been done in high-income countries (HICs). Although they were conducted in LMICs, most of these studies have been conducted in major urban cities,
rather than in remote rural
communities, which represents both a
weakness and an opportunity for the research
and practice of the psychologist and other professionals dedicated
to mental health.
Implications of
ICD-11 MBNDs in public health and its policies
Classification systems have been
criticized for medicalizing common
problems (Stein et al., 2020); however,
the psychopathology subthreshold that is addressed
is relevant for early recognition of future psychiatric disorders –that is, with a focus on primary care (Krasnov, 2021)–.
With the most accurate identification of MBNDs in a country, the availability of assistance services can be evaluated
and plans to implement them can be
structured (Reed, 2021). Furthermore, when combining well-targeted treatment and prevention programs in the field of mental health; and in general,
public strategies, it would be possible to: (a) avoid years lived with disability and deaths, (b) reduce
the stigma associated with mental
disorders, (c) substantially increase social capital, (d) reduce poverty and promote development of a country (Saxena
et al., 2012). When determining what will be financed with a
certain number of resources, the general objective must be to guarantee that health interventions maximize the benefits
for society. For this, evidence-
based prevention programs must be applied to improve positive
mental health (Messias, 2020; Peseschkian
& Remmers, 2020; Sarý & Schlechter, 2020; Smirnova &
Parks, 2018), physical health and
generate economic and social
benefits. In order to favor decision-making in public policies, some issues to be
considered are presented below.
Information systems configure a tool to
improve mental health; however,
difficulties may arise in implementing them due to multiple electronic health records and multiplicity of mental illness classifications.
Many countries have two or more electronic systems
–at least for specialized care units– for registering health information, depending on the state sectors
to which they are attached. An example is the system managed by EsSalud
and the Ministry of Health (MINSA)
in Peru, which are independent
but, in many cases, incompatible.
Another limitation is that there is a group of diagnostic classifications from the WHO and the UN,
to which they must be adjusted as
they offer an international framework for managing, administrating, and researching patients
and services. Making all these classifications compatible allows communication between
healthcare and administrative professionals. It also supports the bases for registering and requesting state
investment for goods and services.
According to Saxena et al. (2012),
ICD-11 MBNDs are mainly linked to four WHO classifications
(in addition to ICD-11 itself) that allow computer management of public health:
(a) the International Classification of Functioning, Disability and Health, (b) the International
Classification of Health Interventions, (c) the International Classification of Primary Care, Third Edition, (d) and the International Classification of External Games of Injury.
In some countries, pilot mapping
studies between clinical
terminologies are being carried out, considering
three layers : (i) Foundation –i. e., a
semantic network of biomedical concepts;
e. g., Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT) and the ICD-11
Foundation Component–, (ii) a formal coding that anchors the meaning
of terms in the semantic web, (iii) Linearization –i. e., a classical tabulation of hierarchical codes that are derived from that network—,
and (iv) Content Model —i. e., an information model of mandatory and optional content, to which each entry in the semantic
network is associated– (Chute & Çelik, 2022).
In the USA, for example, there are
consulting firms Kathy Giannangelo Consulting, LLC and the RXNT compatible software designer corporation, who support the implementation of the ICD-11 clinical codes
to facilitate the billing and reimbursement processes for benefits and medications (e. g., psychotropic
drugs), in addition to training health servers on the classifications of the WHO. However, implementation in developing countries
will require significant effort and
investment (Almeida et al., 2020).
The implementation experiences of the ICD- 11
in countries like Iran (Golpira et al., 2021) and Kuwait
(Ibrahim et al., 2022) can serve as a reference
for other HICs and LMICs in the Latin American
region.
Another aspect to be considered is that
mental health activities in Peru have been usually coded based on health information systems (HIS).
Based on a normative guide (Ministerio de Salud, 2021),
packages are established
(which include the type and quantity of activities) for care and follow-up according to the user’s diagnosis at the different levels
of care. As Hualparuca-Olivera (2022) mentions,
these packages have been prioritized for anxiety, depression, psychosis, and substance use disorders; fact that has limited the clinical management and research of these and other psychopathological
conditions. Moreover, with this
strict rule, diagnosis has often become a sociopolitical consensus to meet health goals (Hualparuca-Olivera, 2022). Although this makes it possible to quantitatively organize the activities and the health budget, it becomes a tedious and unnecessary task for the
healthcare personnel since it fails
to provide quality care and effective
treatment to the user. In this sense, the flexibility offered
by the diagnostic guidelines of the ICD-11 MBNDs to prioritize the
clinician’s criteria could be subtly
transferred to current regulations to improve
the clinical use of the mental health activities proposed
by MINSA.
With the arrival of ICD-11, it is
expected that governments, in coordination with the WHO, or with
its regional entities such as the Pan American Health
Organization, academic societies,
non-governmental organizations would create bridges of communication with
state leaders to establish strategies in order to train each health professionals, administrators and managers on the use of the ICD-11 (Krasnov, 2021; Stein et al., 2020). Likewise, state leaders and their
ministers should organize working
groups to adapt ICD-11 to local laws, policies, health systems and infrastructures, and subsequently design various multilevel actions and train mental health practitioners (Fiorillo & Falkai, 2021). Although educational resources are
available online, the implementation
and training of health professionals (by the Peruvian authorities) has not yet started; and it will take time (R. Valle [Psychiatrist of the National Institute of Mental Health
‘Honorio Delgado-Hideyo
Noguchi’], personal communication, December
1, 2022). Even epidemiological studies
on mental health
in the country are being carried out under the ICD-10 framework. Everything suggests that the implementation of the ICD-11 in Peru will
begin, at least, in a future
five-year period.
Furthermore, since the education of health professionals
represents one of the most essential steps to implement and disseminate the new classification system in routine
care, the WHO International
Advisory Group led by Geoffrey M. Reed has organized
training courses for professionals on the use of the ICD-11 MBNDs chapter
through the GCP Network platform. Likewise,
psychiatric associations, mainly
centralized in Europe and the USA,
have provided educational activities through
interactive virtual formats, including online courses with the active participation of students
through the application of the new guidelines
to clinical cases and discussion of diagnostic dilemmas
(Reed, 2021). Certainly, these trainings
have focused on psychiatrists and at the moment have left aside
other mental health
professionals or those who work on mental health
issues.
Because
ICD-11 will represent
an important change in global clinical practice, it is urgent to promote educational activities to improve the dissemination of this innovative classification approach and contribute to the continuing education of mental
health and related professionals. Also, The WHO Collaborating Centre voor de Familie van Internationale Classificaties in Nederland (WHO-FIC Netwerk; 2019) established a roadmap for the Americas that can be adapted for mental
health issues when implementing ICD-11.
The promotion and dissemination stage, for example, mainly involves (a) designing and strengthening committees, councils
or inter-institutional health
information centers (health
statistics, social security and civil registration);
(b) developing a transition plan and implementation of ICD-10 to ICD-11 aligned
with the country’s health information improvement plan; and (c) develop attractive materials in different formats and use social networks to spread ICD-11 innovations (Fiorillo & Falkai, 2021).
In primary health care (PHC), a large
number of new patients have to be
treated, and certainly the official
version of ICD-11 is not practical. For this
reason, the WHO interested in mental health is in the process of revising the Diagnostic and
Management Guidelines for Mental Disorders in Primary Care 11th revision (ICD-11
PHC). The previous
version (ICD- 10 PHC) included 26 common mental
disorders or relevant to these settings.
The ICD-11 PHC describes
27 mental disorders, 25 of which are equivalent to the ICD-11
MBNDs (Chapman, 2019);
and include problems
with drugs, alcohol,
eating and sleeping, and the body stress syndrome (BSS; see Regier et al., 2020; Robles-García & Reed, 2017). Also, in the ICD-11 PHC, common
presentations in primary care,
distinctive characteristics and relevant differential diagnoses are described; and information for the patient and family, response to both psychological and pharmacological treatment
and indications for referral to a
specialist (Regier et al., 2020). Revisions have also been proposed for mood
and anxiety disorders, BSS, and health anxiety
(HA) proposed for the ICD-11
PHC and suggested that these
categories could be usefully implemented in global primary
care settings (Goldberg et al., 2017).
In PHC, it is important to recognize and intervene in the depressive symptoms that commonly accompany
chronic physical disorders
and the management of multiple somatic symptoms without any accompanying physical illness. According to some authors refer, it is recognized in the ICD-11 PHC that depression
and generalized anxiety disorder (GAD) commonly co-exist, but the diagnostic requirements for depression include a duration of only 2 weeks, while
the requirement for GAD is several months (Razzaque & Minhas, 2018) since the most frequent thing is that a patient
develops anxiety due to his own depressive state condition. This has implications for early management;
since the previous condition
(depression) can be intervened in the first two weeks before
anxiety is generated. Otherwise, a combination of both conditions in clinical thresholds (depression-anxiety) probably leads to comorbidity with other mental
disorders or possible suicide (Regier et al., 2020).
Mixed
states of anxiety
and depressive symptoms
(«cothymia»; see Yang et al., 2022) with
subclinical thresholds are very
common in community settings. For this reason, the WHO Primary
Care Consultative Group recommends three main ways of diagnosis: (a) if there is depressive disorder
(clinical level or
«disorder») + anxiety
disorder (clinical level),
then it is diagnosed as «anxious depression»;
(b) if there is depressive disorder (clinical level) + anxiety disorder
(subclinical level), then it is diagnosed as «depression with current anxiety»; and (c) if there
is depressive disorder (subclinical level) + anxiety
disorder (subclinical level), then it is diagnosed as «subclinical anxious
depression» (see Regier et al., 2020).
Likewise, the ICD-11 Primary
Care Consultation Group evaluated two brief anxiety and
depression screening scales based on
an assembly of the items from the Composite
International Diagnostic Interview
adapted for primary care (CIDI-PC) to help primary care mental health professionals to decide whether
a diagnosable psychological problem was likely to be present (Goldberg et al., 2012). Given
the time and resource pressures –in
addition to patients’ reading comprehension issues– these screening
scales will be especially
useful in LMICs and will be published alongside the ICD-11 PHC (Warren, 2017). The application of these
scales will be soon implemented in all primary care health centers and in mental health care
units within educational institutions
where mental health personnel
work (e. g., school psychologists financed by regional governments) for early detection of negative emotional symptoms. In
addition, it is likely that these
professionals need training in brief cognitive
behavioral interventions to intervene in these cases.
Health
policies for primary
care should also focus on improving the population’s access to mental health services. The need to increase budget for investment in hiring more and better qualified mental health professionals
has been alerted in addition to
improving and increasing primary care services
to achieve better coverage (WHO, 2022a).
Unfortunately, in many LMICs,
specialized care is overwhelmed, and primary
care is very helpful in assisting to ease the
demand for mental health services (Kyanko et
al., 2022; WHO, 2022a). The
importance of improving working
conditions of health professionals for their
own mental well-being in a post-pandemic context has also been highlighted; which also affects
the quality of care in the mental
health services that they offer (Belloni et al., 2022; Shields et al., 2021; WHO, 2022f). The implementation of the ICD-11
MBNDs in primary care should
also consider all these issues.
Mental
disorders are strongly
associated with disability, a term that includes dysfunction of the brain, the body, in your personal
daily activities, and restrictions in your social life. Both physical illnesses and mental disorders have an influence (as a sufficient
or contributing cause) in the disability generation. Disability is often a key factor in:
(a) people seeking
health care; and an important factor in (b) health providers
determining the types of health services
and level of care needed.
However, the frequency, etiology (type of causality), and manifestation of disabilities generated by mental disorders are not well defined
or scientifically studied
(Regier et al., 2020). An attempt has been made to keep
disability out of the main diagnostic
classification of the ICD-11 since it has only incorporated a supplementary
section called the International Classification of Functioning, Disability and Health (ICF). This section
has a disability measurement instrument, WHODAS 2.0, which includes
the following domains: (1) understanding and communication with the
world (cognition); (2) movement and
move (mobility); (3) self-care; (4)
get along with people (interpersonal relationships); (5) home life, occupation, school,
and leisure; and (6) participation in society.
The ICD-11 –like the DSM-5-TR–
has a tradition of incorporating part of the disability construct
for all its disorders, which it names
as «impairment»; which
primarily focuses on social dysfunction. Impairment for each
of the disorders is also accompanied by subjective
«distress»; and for mental disorders that are
dimensionally classified in ICD-11, they define their «severity» (i. e., mild, moderate, or severe). This is where the question arises, why is social dysfunction included in mental disorders
as part of the diagnostic guidelines, unlike the other physical illnesses of the ICD-11? This has to do with scientific and
practical issues since, unlike physical
illnesses, it is very difficult to detect a single (or at least
generalizable) etiology for mental
disorders. Using the guidelines alone, without
including distress or impairment in mental disorders, was shown to lead to high rates of disorder
prevalence; this, without
people generating any personal
or social dysfunction (Regier et al., 2020). Consequently,
it was decided that these two
indicators (distress
and social impairment) constitute the clinical importance of the ICD-11 MBNDs.
According to Saxena et al. (2012), social insurance (financed by state and/or private entities) mainly covers the payment of health services,
distribution of medicines and health devices for a particular patient who pays a monthly
payment. In the event that the
patient cannot pay, a validated disability
certificate is needed so that the insurance continues to be maintained and they continue
to receive decent care. For a
long time in HIC social insurance, the DSM criterion
has been used to regulate
disability criteria, which mainly include:
(a) the existence of a
disorder and (b) that said disorder is associated with significant dysfunction. On the other hand, in most low-income
countries, only people with formal employment are eligible (often
civil servants based in urban
areas), which excludes the working poor and informal and most of the poor rural population. As a result, access to decent and effective treatment was (and continues to be)
conditioned by employment status;
however, most people with a diagnosed mental
disorder are not in the workforce.
In many countries, including Peru, insurers
arbitrarily decide that their financing policies are specific only for some mental disorders. In this sense, insurers focus on the rarest conditions
instead of covering the full range of mental disorders; or include one’s
coverage only for ICD «organic
mental disorders». Therefore, any change in the structure of the ICD-11 MBNDs
with respect to its previous version affects the selection criteria of the beneficiaries
and the conditions of the insurance policy. In fact, with the changes
made in eliminating
«organic» and «non-organic» arbitrary distinction of sleep disorders,
of sexual dysfunctions (even grouped in other chapters of the ICD-11) and
elimination disorders insurers
are likely to adapt their regulations.
The WHO, as already mentioned in the previous section,
has been very clear in emphasizing that disability
should be measured by standard dysfunction domains
–as measured by WHODAS 2.0
and classified by the IFC– and not just by the presence
of a specific diagnosis. For a policy to be inclusive, it will be important that the diagnostic system used to make coverage decisions would also be
inclusive. It is true that no
classification system or instrument is completely free of errors,
and, for this reason, it is of vital importance that the evaluator
is trained, and must also take into account that, like a mental disorder, disability is a dimensional construct, and that a greater biopsychosociocultural
vulnerability must influence temporary or permanent disability.
The evaluation and diagnosis of mental
disorders have always
been part of the forensic
assessment for civil and criminal law. In civil law, it mainly involves tests to specify the effect of emotional
injuries on a third party involved in after a car accident,
guardianship evaluations, ability to write a will, ability to enter into contracts;
testamentary capacity assessments; psychological autopsies in cases of suicide
or sudden death,
fitness for work evaluations; disability insurance benefit assessments
(Saxena et al., 2012). For most of
these situations, the issue at hand
is the determination of the ability to perform
some function, including autonomous decision-making by the person
with a disability. On the other hand,
in criminal law, diagnosis
is usually necessary
for forensic assessments (e. g., of criminal
responsibility and fitness for trial in the offender and assessment of harm in the victim) and for assessments
correctional (e. g., for
prison classification decisions and treatment purposes within the prison system).
The psychopathology constructs offered
in the ICD-11, and as defined by the
WHO, are important issues for the law
in matters of conduct, cognition, will and action in accordance with the understanding of wrongfulness
(García-López, 2022). Consequently, forensic, and correctional evaluators
must address both a legal and mental health
standard since a unified communication code of psychopathology is
needed before the courts of justice
(García-López, 2022; Hall, 2022).
It is crucial to understand
that while forensic
psychology/psychiatry diagnoses behavior, the law typifies
it; In addition, while forensic
psychology bases its knowledge on the ICD-11, the law frames its
action in the codes, norms and statutes
of ministerial entities, international treaties, action protocols of the Supreme Court
of Justice and others. international legal standards (Ramírez
& Dzib, 2022).
With a clinical look at legal
situations, Reed and colleagues
state that some changes in the ICD-11 MBNDs
with respect to their previous version are particularly important in legal matters (see Asociacion Psiquiatrica Mexicana AC, 2022). (a) The
dimensional change that is
established at most in the personality disorder and related traits group must
remove any stigma and deterministic guilt decisions solely based on the presence of traits since not all people are psychopaths
–dissocial traits, which now is
focused on limited pro-social emotions rather than the pattern
of criminal behavior– commit crimes, apart from to the fact that both healthy people and
psychopaths can commit crimes. In
this sense, personality disorder treatment
in legal units can help reduce maladaptive characteristics,
which was previously believed to be impossible or in vain. (b) In the same way, the dimensional change that also affects
the course of the group of schizophrenia or other primary psychotic disorders, explicitly allows the identification of autonomy and awareness of a criminal act without
this necessarily implying a release from criminal responsibility or a permanent stigma. In addition, the condition is prevented from worsening its course if it is intervened early within the civil or criminal units.
(c) The
displacement of the transsexual identity to a chapter outside of mental
disorders collaborates with the
reduction of physical and psychological violence
that these minority groups receive –and seen in legal jurisdictions– due to the double stigma mentioned
above, which are also transferred to prison where they are often tortured. (d) The
inclusion of complex PTSD as a
diagnostic category helps to quantify
the psychic damage to penalize the guilty party of producing a trauma (with internal disorganization) in the victim; what could not be done before because
the diagnosis was confused with borderline personality disorder. (e) Paraphilic disorders in ICD-11 do not require the commission of an act in response to sexual desires
(e. g., 6D32 pedophilic disorder, 6D33 coercive sexual sadism disorder, etc.) to be diagnosed. This allows early detection and intervention of these mental
disorders before the crime is
committed without the need to stigmatize these people.
However, from a legal perspective, as Münch et al. (2020) mention, ICD-11
may have some negative implications for forensic assessment. Specifically, in groups of disorders mainly described as
«behavior harmful to others» –e. g., Disruptive behavior or dissocial
disorders and Paraphilic disorders (excluding consensual behaviors) or–, since using the conjunction
«or» is grouped
in the same category to patients who have
distress/deterioration with individuals who act recurrently harming others. These patterns «without prosocial
emotions» in criminal behavior,
–which may be due to «learned
and self-consensual vices,
and not due to mental disorders–, are the ones that most predict recidivism and a rejection of prison treatment (Münch et
al., 2020). Bründl and Fuss (2021), reinforce the argument that the continuity of intermittent explosive disorder and compulsive sexual behavior in ICD-11 is still questionable –although, other authors mention that the
continuity of compulsive sexual behavior promote research and improvement in prevention and treatment (Mead & Sharpe, 2019)–. In addition, including harm to other people’s health as one of the
criteria for substance use could medically
justify crimes committed under the influence of alcohol or drugs (García-López, 2022;
Reed et al., 2019).
As evidenced, there
is a lot of misinformation and lack of
understanding between clinical and legal disciplines when mental health problems are involved in criminal behavior. Most criminal liability decisions only
consider schizophrenia as a defense
since criminal behavior is attributed as the effect
of the individual’s lack of awareness
when differentiating the illegality of its acts; and only in some severe and comorbid
cases,
the other disorders that affect the lack of emotional regulation are considered as defenses. In
this sense, it is clear, as mentioned by Saxena et al. (2012),
that a diagnosis of a mental
disorder in a defendant does not imply by itself being exculpatory or mitigating, or decisive
for the certain prognosis of recidivism; however, it is used to communicate the
results of an expertise
to the judge or legal actors, and to make legal decisions regarding mental treatment
within civil or criminal units. Criminal responsibility and the capacity to stand trial will always have to be
based on a deep and ideographic expertise of conscience and volitional control rather than on a psychiatric diagnosis (Carroll et al., 2022).
This issue is not often well understood
by legal professionals, who seek a deterministic standard
framework to establish
a cause for penance; however,
ICD-11 has been designed
to communicate and treat health problems. In this sense,
the implications of the changes in the ICD-11 MBNDs must be carefully analyzed in order to
adapt to the standards already used
in legal contexts. If there is no
rigorous training in mental health issues and in national and international standards for justice
administrators or health professionals –who work in these legal units–,
it is possible that corruption, impunity, negligence, abuse, and injustice continue to reign in
these contexts.
Keeley (2016) states that classifications of mental disorders represent a necessary evil, as
they provide the infrastructure to help people with mental problems (i. e., clinical
use). In other words, they make it possible to have an exhaustive and consensual list of each of people’s
problems. With an adequate diagnosis,
tracking the social
and personal burden
of the patient, the following
are ideally improved: (a) communication between professionals, (b) the standardized identification of clinical
conditions for research and (c) the choice of best treatments (Keeley, 2016).
The ICD-11 has been committed to mental health, and its inclusive perspective with states
with fewer resources focused
on prevention represents one of its strongholds.
While the interest and benefits to be generated
by such an approach are laudable, such a prospect
may also bring some limitations. Since the reliability and validity of the diagnoses is improved, it allows
to reach the objective of improving
communication between health professionals. Although the ICD-11 MBNDs guidelines are flexible
at the clinician’s criterion, which improves their cross-cultural applicability, this may somewhat decrease its reliability for research compared to the DSM-5 TR. This system, and other dimensional classification frameworks, due to the competence they represent, have also contributed
(e. g., with the lifespan and
stepwise approach) to improving
the validity and reliability of the diagnostic categories of the ICD-11 MBNDs in research and in specialized care. In short,
this reflects the current knowledge of the
organization; and the changes and additions of the ICD-11
MBNDs.
However, there are gaps regarding its
usefulness for the most appropriate psychological
and psychiatric treatment for the individual
needs of the user. This is
due to the phenomenological and non-etiological nature of said diagnoses; besides, it does not consider the subjective experience, the strengths of the human
being; instances that are inseparable from the general
functioning –i. e., positive,
normal (adapted) or pathological
ones– of the patient. In this sense, the psychologist’s work for the diagnosis, prognosis, treatment, and follow-up of the patient’s clinical condition will be preliminarily based on
the ICD-11 classification, but it will not be usually limited
to the latter. The conceptualization of the case,
through the different psychological frameworks
(including the stepwise
approach and a biopsychosociocultural view of the underlying factors), will be an essential tool for clinical
management from psychological practice.
The implications for public health and
its policies for the implementation of the ICD-11
MBNDs lie in the adaptability of current information systems and
their regulations to improve the clinical use of these diagnoses. A considerable economic
investment and continuous training of health
care and administrative servers will be necessary to better understand the reasons, content, and opinions of the
changes in this eleventh
revision. Other important aspects derived from the
above are: (a) the management of
ICD-11 MBNDs in primary
care, which implies
early identification of the
most common mental conditions (Regier et al., 2020), and the creation of more establishments and the improvement of the conditions in employment contracts of human resources (see Hualparuca-Olivera, 2022);
(b) disability assessment for health insurance financing issues will have to focus more on personal
and social dysfunction than on the ICD-11 MBNDs themselves;
(c) in legal environments,
there will be little impact of this
new model for civil and criminal law.
The benefits will be consolidated to a greater extent if communication between legal actors and mental health professionals
is improved, thereby reducing the
stigma associated with mental disorders for the commission of the crime.
It is unfortunate that the field studies
carried out by the WHO for the
revision and implementation of the ICD-11
have not included
Peru or other
Spanish- speaking South American countries. In addition, it
is important to consider studies
that evaluate the applicability
and clinical use, as well as the clinical management perspectives of the different
mental health professionals
perceived by the health professionals
themselves and the users. Likewise, it is
important to consider in epidemiological studies other common but misdiagnosed conditions (e. g., personality
disorder) since this will provide a better overview of mental health in Peruvians. Finally, experimental research
(randomized clinical trials)
of brief psychological interventions
is necessary to prove its
efficacy and efficiency, and to compare to other evidence-based treatments.
The review and analysis presented in
this article can serve as an additional resource for comprehensive training
on the ICD-11 MBNDs by describing the science-practice-public
policy triad from the psychology
perspective. This resource can also
be considered by other professionals who have
previous knowledge in mental health and work closely on
this topic since it uses terminology
compatible with other health sciences
(psychiatric medicine, nursing). Moreover, the previously described implications can be
of reflection and value for professionals in the social sciences
(i. e., social workers)
and administrative sciences (health managers and telehealth or digital health consultants) and legal sciences (forensic psychiatrists and
psychologists, judges, etc.) linked
to mental health; a fact that as a whole also represents a great tool for
decision-making in public
policies related to mental health.
We declare that we have no conflict of interest.
In this research,
no experiments have been carried out on humans or animals, nor
conducts that come into conflict
with ethical issues because it is a theoretical paper.
The authors participated equally in the preparation of this paper.
We thank the reviewers for their comments
on our paper for its improvement.
Almeida, M. S. C., Sousa-Filho, L. F., Rabelo, P. M., & Santiago, B. M. (2020).
International Classification of Diseases – 11th revision:
From Design to Implementation.
Revista de Saúde Pública, 54,
104. https://doi.org/10.11606/S1518-8787.2020054002120
Alves, L. E., Monteiro, B. M. M., &
Souza, J. C. (2020). Comparison
of the Classification of Child Development Disorders Using DSM-5, ICD-10 and ICD-11. Research,
Society and Development, 9(10), e6579109058-e6579109058. https://doi.org/10.33448/RSD-V9I10.9058
American
Psychiatric Association. (2022). Diagnostic
and Statistical
Manual of Mental Disorders (5th ed., text revision). American Psychiatric Publishing.
Appelbaum, P. S. (2017). Moving Toward the Future in the Diagnosis of Mental Disorders. Psychological Science
in the Public Interest, 18(2),
67-71. https://doi.org/10.1177/1529100617727267
Arntz, A., Mensink, K., Cox, W. R., Verhoef, R. E.
J., Van Emmerik, A. A. P., Rameckers, S. A., Badenbach, T., & Grasman, R. P. P. P. (2022). Dropout from Psychological Treatment for Borderline Personality Disorder: A Multilevel Survival Meta-Analysis. Psychological Medicine, 53(3), 668-686.
https://doi.org/10.1017/S0033291722003634
Bach, B., Bo, S., & Keeley, J. W. (2022). Diagnostic Systems and Models: DSM-5 Criteria,
ICD-11 Guidelines, and Dimensional
Horizons. In G. J. G. Asmundson (Ed.), Comprehensive Clinical Psychology (2nd
ed., pp. 36- 58). Elsevier.
https://doi.org/10.1016/B978-0-12-818697-8.00111-4
Bach, B., & Simonsen, S. (2021). How
does Level of Personality Functioning
Inform Clinical Management and Treatment? Implications for ICD-11 Classification of Personality Disorder Severity. Current Opinion in Psychiatry, 34(1),
54-63. https://doi.org/10.1097/YCO.0000000000000658
Baleige,
A., De la Chenelière, M., Dassonneville,
C., & Martin, M. J. (2022).
Following ICD-11, Rebuilding Mental
Health Care for Transgender Persons: Leads from Field Experimentations in Lille, France. Transgender
Health, 7(1), 1-6. https://doi.org/10.1089/trgh.2020.0143
Balling, C. E., South, S. C., Lynam, D. R., & Samuel, D. B. (2023). Clinician Perception
of the Clinical Utility of the Hierarchical Taxonomy of Psychopathology (HiTOP) System. Clinical Psychological Science, 0(0). https://doi.org/10.1177/21677026221138818
Belloni, M., Carrino, L., &
Meschi, E. (2022).
The Impact of Working Conditions on Mental Health:
Novel Evidence from the UK. Labour Economics, 76, 102176. https://doi.org/10.1016/j.labeco.2022.102176
Bründl, S., & Fuss, J. (2021). Impulskontrollstörungen in der ICD-11 [Impulse control disorders in the ICD-11]. Forensische Psychiatrie, Psychologie, Kriminologie, 15(1), 20-29. https://doi.org/10.1007/s11757-020-00649-2
Carroll, A., Walvisch, J., & Marsh, T. (2022). Personality Disorders and Forensic Assessments: The Benefits of ICD-11. Medicine, Science and the Law. Advanced Online Publication. https://doi.org/10.1177/00258024221094188
Caux-Harry, R. (2018, June 27). It is Coming: ICD-11 Released. In
3M Inside Angle. https://insideangle.3m.com/his/blog-post/it-is-coming-icd-11-released
Chapman, S. (2019, June 28). Clinical Descriptions and Diagnostic Guidelines (CDDG) for ICD 11
Mental, Behavioural
and Neurodevelopmental Disorders. Dx Revision Watch.
https://wp.me/pKrrB-4IQ
Chute, C. G., & Çelik,
C. (2022). Overview of ICD-11 Architecture and Structure. BMC Medical
Informatics and Decision
Making, 21(6),
378. https://doi.org/10.1186/s12911-02-01539-1
Columbia Psychiatry. (2022, February 4).
Why There Are Two Classification Systems in Psychiatry and How They
Differ. [Video]. Youtube. https://www.youtube.com/watch?v=aHL4rWUEuYg
Conway, C. C., Forbes, M. K., &
South, S. C. (2021). A Hierarchical Taxonomy of Psychopathology (HiTOP). Primer for Mental Health Researchers. Clinical Psychological
Science, 10(2), 236-258. https://doi.org/10.1177/21677026211017834
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The Impact of Mental Illness
Stigma on Seeking
and Participating in Mental
Health Care. Psychological Science in the Public Interest, 15(2), 37-70. https://doi.org/10.1177/1529100614531398
Evans, S. C., Reed, G. M., Roberts, M. C., Esparza,
P., Watts, A. D., Correia, J. M., Ritchie, P., Maj, M., & Saxena, S. (2013). Psychologists’
Perspectives on the Diagnostic Classification of Mental Disorders: Results
from the WHO-IUPsyS Global Survey. International Journal of Psychology, 48(3), 177-193.
https://doi.org/10.1080/00207594.2013.804189
File, T., & Marlay, M. (2022). Regardless of household type, LGBT adults struggled more
with mental health than non-LGBT adults.
In US Census Bureau. https://www.census.gov/library/stories/2022/06/lgbt-adults-report-anxiety-depression-during-pandemic.html
Fiorillo,
A., & Falkai,
P. (2021). The ICD-11 is Coming to
Town! Educational Needs, Paradigm Shifts and Innovations in Mental Health
Care Practice. European Psychiatry, 64(1),
73. https://doi.org/10.1192/J.EURPSY.2021.2254
First,
M. B., Gaebel, W., Maj, M., Stein, D. J., Kogan, C. S.,
Saunders, J. B., Poznyak, V. B., Gureje, O., Lewis-
Fernández, R., Maercker, A., Brewin,
C. R., Cloitre, M., Claudino, A., Pike, K. M., Baird, G., Skuse, D., Krueger, R. B., Briken, P., Burke, J. D., … Reed, G. M. (2021). An Organization- and Category-Level Comparison of Diagnostic
Requirements for Mental Disorders in ICD- 11 and DSM-5. World Psychiatry, 20(1), 34-51. https://doi.org/10.1002/WPS.20825
Gaebel, W., & Kerst, A. (2019). ICD-11 Mental, Behavioural or Neurodevelopmental
Disorders: Innovations and Managing
Implementation. Archives
of Psychiatry and Psychotherapy,
21(3), 7-12. https://doi.org/10.12740/APP/111494
Gaebel,
W., Stricker, J., & Kerst, A. (2022). Changes from ICD-10 to ICD-11 and Future Directions in Psychiatric Classification. Dialogues in Clinical Neuroscience, 22(1),
7-15. https://doi.org/10.31887/DCNS.2020.22.1/WGAEBEL
García-López, E. (2022). CIE-11 y Psicopatología forense para el sistema de justicia en América Latina
[ICD-11 and Forensic Psychopathology for the Justice System in Latin
America]. https://doi.org/10.13140/RG.2.2.10896.28165
Garralda, E. (2016). ICD-11-Comparison with DSM-5 and Implications for Child & Adolescent Psychiatric Disorders. In M. Hodes & S. Gau (Eds.),
Positive Mental Health,
Fighting Stigma and Promoting Resiliency for Children and Adolescents (pp.
15-35). Academic Press. https://doi.org/10.1016/B978-0-12-804394-3.00002-4
Garralda, E. (2021). ICD 11 Through the Lens of Child and Adolescent
Psychiatry. https://bupnet.dk/wp-content/uploads/2021/06/1-EG-Denmark-ICD-11-DS-June- 20215377.pdf
Gelezelyte,
O., Kvedaraite, M., Kairyte,
A., Roberts, N. P., Bisson,
J. I., & Kazlauskas, E. (2022). The Mediating
Role of Complex Posttraumatic Stress and Borderline Pattern
Symptoms on the Association Between Sexual Abuse and Suicide Risk. Borderline
Personality Disorder and Emotion Dysregulation, 9(1), 13. https://doi.org/10.1186/s40479-022-00183-z
Goldberg, D. P., Lam, T.-P., Minhas, F.,
Razzaque, B., Robles,
R., Bobes, J., Iglesias, C., Fortes, S., Mari, J. de J.,
Gask, L., García, J. Á., Dowell, A. C., Rosendal, M., & Reed, G. M. (2017).
Primary Care Physicians’ Use of the Proposed Classification of Common
Mental Disorders for ICD-11.
Family Practice, 34(5), 574-580.
https://doi.org/10.1093/fampra/cmx033
Goldberg, D. P., Prisciandaro, J. J., & Williams,
P. (2012). The Primary Health Care Version of
ICD-11: The Detection of Common
Mental Disorders in General Medical Settings. General Hospital
Psychiatry, 34(6),
665-670. https://doi.org/10.1016/j.genhosppsych.2012.06.006
Golpira, R., Azadmanjir, Z., Zarei, J., Hashemi, N., Meidani, Z.,
Vahedi, A., Bakhshandeh,
H., Fakharian, E., & Sheikhtaheri, A. (2021).
Evaluation of the Implementation of
International Classification of
Diseases, 11th Revision for
Morbidity Coding: Rationale and Study Protocol. Informatics in Medicine
Unlocked, 25, 100668. https://doi.org/10.1016/J.IMU.2021.100668
Gozi,
A. (2019). Highlights of ICD-11 Classification of Mental, Behavioral, and Neurodevelopmental Disorders. Indian
Journal of Private Psychiatry, 13(1),
11-17. https://doi.org/10.5005/JP-JOURNALS-10067-0030
Graham, D. M. (2019). Non-Conforming, Part 1: ICD-11. The Lancet Psychiatry, 6(6), 470-471.
https://doi.org/10.1016/S2215-0366(19)30168-3
Guggenheim, F. G. (2013).
Public Health Aspects of Diagnosis
and Classification of Mental and Behavioral Disorders: Refining the Research Agenda
for DSM-5 and ICD-11.
The Journal of Clinical Psychiatry, 74(7),
e664. https://doi.org/10.4088/JCP.13BK08586
Gureje, O., Lewis-Fernandez,
R., Hall, B. J., & Reed, G. M. (2020). Cultural Considerations in the Classification of Mental Disorders: Why and How in ICD-11. BMC Medicine, 18(1), 1-2. https://doi.org/10.1186/S12916-020-1493-4
Hall, H. V.
(2022). Criminal- and Civil-Forensic Factors
in a Methamphetamine Murder
Case. In H. V. Hall & J. G. Poirier (Eds.), Forensic Psychology
and Neuropsychology for Criminal and Civil Cases (2nd ed.). CRC Press.
https://doi.org/I0.4324/9781003213307
Harrison, J. E., Weber, S., Jakob, R., & Chute, C. G. (2021). ICD-11:
An International Classification of
Diseases for the
Twenty-First Century. BMC Medical
Informatics and Decision Making, 21(6), 1-10. https://doi.org/10.1186/s12911-021-01534-6
Herpertz, S. C., Schneider, I., Renneberg, B., & Schneider,
A. (2022). Patients
with Personality Disorders
in Everyday Clinical Practice. Dtsch Arztebl International, 119(1-2),
1-7. https://doi.org/10.3238/arztebl.m2022.0001
Hooley, J. M., Nock, M. K., &
Butcher, J. N. (2021). Abnormal Psychology (18th
ed., pp. 77-119). Pearson Education Limited.
Hualparuca-Olivera, L. (2022). Cultural Lenses of the Utility of
the ICD-11-PD Model: Integrating the Peruvian
Context. Frontiers Psychiatry, 13,
1016471. https://doi.org/10.3389/fpsyt.2022.1016471
Hualparuca-Olivera,
L., Ramos Campos, D. N., Arauco Vivas, P. A., & Coz, R. M. (2022).
Integrative Dimensional Personality Inventory for ICD-11:
Development and Evaluation
in the Peruvian Correctional
Setting. Liberabit, 28(1), e540. https://doi.org/10.24265/liberabit.2022.v28n1.05
Hyeji, K., Doyeon, A., Yeojin, L., and Hyekyung, W. (2022). An overview
and future challenges of the WHO International Classification of Disease ICD-11.
J
Heal. Info Stat,
47(4), 241-249. https://doi.org/10.21032/jhis.2022.47.4.241
Ibrahim, I., Alrashidi, M., Al-Salamin, M., Kostanjsek, N., Jakob, R., Azam, S., Al-Mazeedi, N., & Alasoomi, F. (2022). ICD-11 Morbidity Pilot in Kuwait: Methodology and Lessons Learned
for Future Implementation. International Journal of
Environmental Research and Public
Health, 19(5), 3057. https://doi.org/10.3390/IJERPH19053057
Iliakis,
E. A., Ilagan, G. S., & Choi-Kain, L. W. (2021). Dropout Rates from Psychotherapy Trials for Borderline
Personality Disorder: A Meta-Analysis. Personality Disorders:
Theory, Research,
and Treatment, 12(3),
193-206. https://doi.org/10.1037/PER0000453
Instituto Nacional de Salud Mental.
(2019). Estudio epidemiológico de salud mental en hospitales regionales - 2015 [Epidemiological
Study of Mental Health in
Regional Hospitals - 2015]. https://www.insm.gob.pe/investigacion/archivos/estudios/2020/VolXXXV2019Nro1EESMenHospitalesRegionales.pdf
Kamenov,
K., Twomey, C., Cabello, M., Prina, A. M., & Ayuso-Mateos, J. L. (2017). The Efficacy of Psychotherapy, Pharmacotherapy and their Combination on Functioning and Quality of
Life in Depression: A Meta-Analysis. Psychological Medicine, 47(3), 414-425.
https://doi.org/10.1017/S0033291716002774
Keeley, J. W. (2016). Improving the Clinical Utility of Mental Disorder Classifications.
Division 12 of the American Psychological Association. https://div12.org/improving-the-clinical-utility-of-mental-disorder- classifications/
Keeley, J. W., Reed, G. M., Roberts, M.
C., Evans, S. C., Medina-Mora, M.
E., Robles, R., Rebello, T., Sharan, P.,
Gureje, O., First, M. B., Andrews, H. F., Ayuso- Mateos, J. L., Gaebel, W., Zielasek, J., & Saxena, S. (2016). Developing a Science of Clinical Utility in Diagnostic Classification Systems Field Study Strategies
for ICD-11 Mental and Behavioral
Disorders. The American Psychologist, 71(1), 3-16. https://doi.org/10.1037/a0039972
Kielkiewicz, K. (2019).
Consequences of the Lack of Focus on the Aetiology of Mental Disorders
in the Psychiatric Perspective of Mental Health.
In K. Kielkiewicz (Ed.), Psychological Perspectives on Health and Disease,
vol. 2. Manifestation and Diagnoses of Health Conditions (pp. 4-10). University of Economics and Human Sciences Press. https://doi.org/10.5709/PPHD-2-1
Kountouras, G., & Sotirgiannidou, K. (2022). Psychodiagnostic
Classification Systems: A Critical View. International Journal of Social Science Research
and Review, 5(4), 30-40. https://doi.org/10.47814/IJSSRR.V5I4.226
Kramer, U., Eubanks, C. F., Bertsch, K.,
Herpertz, S. C., McMain, S., Mehlum, L., Renneberg, B., & Zimmermann, J. (2022). Future Challenges
in Psychotherapy Research for Personality Disorders. Current Psychiatry Reports, 24(11), 613-622. https://doi.org/10.1007/s11920-022- 01379-4
Kramer,
U., Ranjbar, S., & Caspar,
F. (2022). Using
Case Formulation for Prediction of the Therapeutic Alliance
in Treatment for Borderline Personality Disorder. Personality
Disorders. https://doi.org/10.1037/per0000555
Krasnov, V. N. (2021). ICD-11 as a Paradigm Shift Phase in the Classification of Mental
Disorders. Consortium Psychiatricum,
2(2), 72-75. https://doi.org/10.17816/CP70
Krawczyk, P., & Swiecicki, L. (2020). ICD-11 vs. ICD-10 - a review of updates and novelties introduced in the latest
version of the WHO International Classification of
Diseases. Psychiatria Polska, 54(1), 7-20. https://doi.org/10.12740/PP/103876
Kring, A. M., & Johnson, S. L. (2021).
Abnormal Psychology: The Science and Treatment
of Psychological Disorders (15th ed.). John Wiley & Sons, Inc.
Kulygina,
M. A., Syunyakov, T. S., Fedotov,
I. A., & Kostyuk, G. P. (2021). Toward ICD-11
Implementation: Attitudes and expectations of the Russian Psychiatric
Community. Consortium Psychiatricum,
2(2), 23-34. https://doi.org/10.17816/CP80
Kyanko,
K. A., A. Curry, L., E. Keene, D.,
Sutherland, R., Naik, K., & Busch, S. H. (2022). Does Primary Care Fill the Gap in Access to Specialty Mental Health Care? A Mixed Methods Study. Journal of General Internal Medicine, 37(7), 1641-1647. https://doi.org/10.1007/s11606-021-07260-z
Leichsenring, F., Steinert, C., Rabung, S., & Ioannidis, J. P. A. (2022). The Efficacy of
Psychotherapies and Pharmacotherapies for Mental Disorders in Adults: An Umbrella Review and Meta-Analytic Evaluation of Recent Meta-Analyses. World Psychiatry, 21(1), 133-
145. https://doi.org/10.1002/WPS.20941
Lindmeier, C. (2022). WHO’s New International Classification
of Diseases (ICD-11) Comes Into Effect.
Pan American Health Organization. https://www.paho.org/en/news/11-2-2022-whos-new-international-classification-diseases-icd-11-comes-effect
Lindmeier, C., & Joi, P. (2018). WHO Releases New International Classification of Diseases
(ICD-11). Pan American
Health Organization. https://www.paho.org/en/news/11-2-2022-whos-new-international-classification-diseases-icd-11-comes-effect
Livesley, W. J. (2018). Integrated Modular
Treatment. In W. J. Livesley & R. Larstone
(Eds.), Handbook of Personality Disorders: Theory, Research,
and Treatment (pp. 645-673). The Guilford Press.
Maercker,
A. (2022). The ICD-11 Diagnoses in the Mental Health Field – An Innovative Mixture.
Clinical Psychology in Europe, 4(Special
Issue), Article e10647. https://doi.org/10.32872/cpe.10647
Mead, D., &
Sharpe, M. (2019). Pornography and sexuality research papers
at the 5th International Conference on Behavioral
Addictions. Sexual Addiction & Compulsivity, 25(4), 248-268. https://doi.org/10.1080/10720162.2019.1578312
Menon, G. R.,
Yadav, J., Aggarwal, S., Singh, R., Kaur, S., Chakma, T., Periyasamy, M., Venkateswaran, C., Singh,
P.
K., Balachandar, R., Kulkarni,
R., Grover, A., Mishra,
B. K., Viray, M., Devi, K. R., Singh,
K. H. J., Saha, K. B., Barde, P.
V, Thomas, B., … Panda, S. (2022). Psychological Distress and Burnout Among Healthcare
Worker During COVID-19 Pandemic in India - A Cross- Sectional Study.
PLOS ONE, 17(3),
e0264956. https://doi.org/10.1371/JOURNAL.PONE.0264956
Messias,
E. (2020). Positive Psychiatry: An Introduction. In E. Messias, H. Peseschkian & C. Cagande
(Eds.), Positive Psychiatry, Psychotherapy and Psychology: Clinical
Applications (pp. 3-9). Springer Nature Switzerland
AG. https://doi.org/10.1007/978-3-030-33264-8_1
Michelini, G., Palumbo, I. M., DeYoung, C. G., Latzman, R. D.,
& Kotov, R. (2021). Linking RDoC and HiTOP: A New Interface for Advancing Psychiatric Nosology and
Neuroscience. Clinical Psychology Review, 86, 102025. https://doi.org/10.1016/J.CPR.2021.102025
Miles, L. (2018). Diagnosing
and Classifying Psychological Disorders. OpenStax;
Hostos Community College
Library. https://guides.hostos.cuny.edu/psy142/2-1
Ministerio de Salud. (2011).
Norma técnica de salud «Categorías de establecimientos del sector salud» [Technical
health standard ‘Categories of Health Sector Establishments’]. (RMN°
546-2011-MINSA). https://www.gob.pe/institucion/minsa/normas-legales/243402546-2011-minsa
Ministerio de Salud. (2021). Manual de registro y codificación de actividades en la atención salud de salud mental:
Sistema de información HIS [Manual for Registration and Coding of activities in mental health care: HIS Information System]. https://www.gob.pe/institucion/minsa/informes-publicaciones/3249452-manual-de-registro-y-codificacion-de-actividades-en-la-atencion-salud-de-salud-mental-sistema-de-%20informacion-his
Mulder, R. T. (2012). Why we Need a New Classification of Personality Disorders. https://doi.org/10.3389/fpsyt.2021.655548
Münch, R., Walter, H., & Müller, S. (2020). Should Behavior Harmful to Others be a
Sufficient Criterion of Mental Disorders?
Conceptual Problems of the Diagnoses of Antisocial Personality Disorder and Pedophilic Disorder. Frontiers
in Psychiatry, 11, 954. https://doi.org/10.3389/fpsyt.2020.558655
O’Brien, E. (2022). Major Diagnostic Differences Between DSM-5 and ICD-11. Psychiatric Times. https://www.psychiatrictimes.com/view/major-diagnostic-differences-between-dsm-5-and-icd-11
Paniagua, F. A.
(2018). ICD-10 versus DSM-5 on Cultural Issues:
SAGE Open, 8(1). https://doi.org/10.1177/2158244018756165
Patel,
K., Caddy, C., & Tracy,
D. K. (2017). Who do they think we are? Public perceptions of
psychiatrists and psychologists. Advances in Mental Health, 16(1), 65- 76. https://doi.org/10.1080/18387357.2017.1404433
Peseschkian, H., & Remmers, A. (2020). Positive
Psychotherapy: An Introduction. In E. Messias,
H. Peseschkian, & C. Cagande (Eds.), Positive
Psychiatry, Psychotherapy and Psychology: Clinical Applications, (pp. 11-32). Springer Nature Switzerland AG. https://doi.org/10.1007/978-3-030-33264-8_2
Peterson, C. (2009). Psychological Approaches to Mental
Illness. In T. L. Scheid & T. N. E. Brown (Eds.), A Handbook for the Study of Mental Health: Social
Contexts, Theories, and Systems (2nd ed., pp. 89-105). Cambridge University Press. https://doi.org/10.1017/CBO9780511984945.008
Pezzella, P. (2022). The ICD-11 is Now Officially in Effect. World Psychiatry, 21(2),
331-332. https://doi.org/10.10 02/wps.20982
Quiroz-Valdivia, R., Chávez-Gonzales,
W., & Holgado-
Canales, M. (1997). Estructura y contenido del síndrome esquizofrénico del
hombre andino de la subregión
Cusco (Perú) [Structure and Content of the Schizophrenic Syndrome of the Andean Man of the Cusco
Subregion (Peru)]. Situa, 5(10).
https://sisbib.unmsm.edu.pe/Bvrevistas/situa/1997_n10/sesquizofrenico.htm
Ramírez, P. G., & Dzib, J. P. (2022). Errores
en los dictámenes psicológicos
forenses (impacto en la memoria, falsos positivos, falsos negativos) [Errors in Forensic
Psychological Opinions (Impact on Memory, False Positives, False Negatives)]. South Florida
Journal of Development, 3(2), 2643-2660. https://doi.org/10.46932/sfjdv3n2-084
Razzaque, B., & Minhas,
F. A. (2018). International Classification
of Diseases-11: Primary Care
Perspective. Indian Journal of Social Psychiatry, 34(5), 75-78.
https://doi.org/10.4103/IJSP.IJSP_77_17
Reed, G. M. (2010). Toward ICD-11: Improving the Clinical Utility
of WHO’s International Classification of Mental Disorders. Professional Psychology: Research and Practice, 41(6), 457-464.
https://doi.org/10.1037/A0021701
Reed, G. M. (2021). An Introduction to ICD-11 Mental, Behavioural and Neurodevelopmental Disorders: Summary and Close. https://www.rcpsych.ac.uk/docs/default-source/events/development/icd-11/calc-g-1.pdf?sfvrsn=edd2f1ab_4
Reed, G. M., First, M. B., Billieux, J., Cloitre, M., Briken, P., Achab, S., Brewin,
C. R., King, D. L., Kraus, S. W., &
Bryant, R. A. (2022). Emerging Experience with Selected New Categories in the ICD-11:
Complex PTSD, Prolonged
Grief Disorder, Gaming Disorder, and Compulsive Sexual Behaviour Disorder. World Psychiatry, 21(2), 189-213. https://doi.org/10.1002/WPS.20960
Reed, G. M., First, M. B., Kogan, C. S., Hyman, S. E., Gureje,
O.,
Gaebel, W., Maj, M., Stein, D. J., Maercker, A., Tyrer, P., Claudino, A., Garralda, E., Salvador-Carulla, L., Ray, R., Saunders,
J. B., Dua, T., Poznyak, V., Medina-Mora,
M. E., Pike, K. M., … Saxena, S. (2019). Innovations and Changes in the ICD-11 Classification of Mental, Behavioural and
Neurodevelopmental Disorders. World Psychiatry, 18(1), 3-19. https://doi.org/10.1002/WPS.20611
Reed, G. M., Keeley, J. W., Rebello, T. J., First, M. B., Gureje,
O.,
Ayuso-Mateos, J. L., Kanba, S., Khoury,
B., Kogan, C. S., Krasnov, V. N., Maj, M., de Jesus Mari, J., Sharan, P., Stein, D. J., Zhao, M.,
Akiyama, T., Andrews, H. F., Asevedo, E., Cheour, M., … Medina-Mora, M. E. (2018). Clinical Utility of ICD-11 Diagnostic Guidelines for High-Burden Mental Disorders: Results
from Mental Health Settings in 13 Countries. World Psychiatry, 17(3), 306-315. https://doi.org/10.1002/WPS.20581
Reed, G. M., Sharan, P., Rebello, T. J., Keeley, J. W., Elena Medina-Mora, M., Gureje, O., Luis Ayuso-Mateos, J., Kanba, S., Khoury, B., Kogan, C. S., Krasnov,
V. N.,
Maj,
M., de Jesus Mari, J., Stein, D. J., Zhao, M.,
Akiyama, T., Andrews, H. F., Asevedo, E., Cheour, M.,… Pike, K. M. (2018). The ICD-11 Developmental Field Study of Reliability of Diagnoses of High-Burden Mental
Disorders: Results Among Adult Patients
in Mental Health Settings
of 13 Countries. World Psychiatry,
17(2), 174-186. https://doi.org/10.1002/wps.20524
Regier,
D. A., Goldberg, D. P., Üstün, B. T., & Reed, G. M. (2020). DSM-5 and ICD-11
classifications. In J. R. Geddes,
N. C. Andreasen, & G. M. Goodwin (Eds.), New Oxford
Textbook of Psychiatry (3th ed., pp. 51-61). Oxford
University Press.
Robles-García, R., & Reed, G. M. (2017). WHO’s ICD-11 for Primary Health Care. Salud Mental, 4(2), 45-46. https://doi.org/10.17711/SM.0185-3325.2017.006
Robles, R., De la Peña, F. R., Medina-Mora, M. E., Márquez- Caraveo,
M. E. de los D., Domínguez, T., Juárez, F., Rojas, A. G., Sarmiento-Hernández, E. I., Feria, M., Sosa, L., Aguerre, R. E., Ortiz,
S., Real, T., Rebello, T., Sharan, P.,
& Reed, G. M. (2021). ICD-11
Guidelines for Mental and Behavioral Disorders of Children and Adolescents: Reliability and Clinical Utility. Psychiatric Services, 73(4),
396-402. https://doi.org/10.1176/APPI.PS.202000830
Roessner, V., Ehrlich, S., & Vetter, N. C. (2016). Child and Adolescent Psychiatry in
ICD-11: An Opportunity to Overcome
Mistakes Made in DSM-5?
European Child &
Adolescent Psychiatry, 25(9),
935-938. https://doi.org/10.1007/S00787-016-0894-6
Sarý,
T., & Schlechter, A. D. (2020). Positive Psychology: An Introduction. In E. Messias, H. Peseschkian, & C. Cagande
(Eds.), Positive Psychiatry, Psychotherapy and Psychology: Clinical Applications (pp.
33-46). Springer Nature Switzerland
AG. https://doi.org/10. 1007/978-3-030-33264-8_3
Saxena, S., Esparza, P., Regier, D. A., Saraceno, B.,
& Sartorius, N. (2012). Public Health Aspects of Diagnosis and Classification of Mental and Behavioral
Disorders: Refining the Research Agenda for DSM-5 and ICD-11. American Psychiatric Association.
Seligman, M. E. P.
(2019). Positive Psychology: A
Personal History. Annual Review of Clinical
Psychology, 15(1),
1-23. https://doi.org/10.1146/annurev-clinpsy-050718-095653
Semple, D., & Smyth, R. (2019). Oxford Handbook of Psychiatry (4th ed.).
Oxford University Press.
Sharan, P., & Hans, G. (2021).
Cultural Issues Related to ICD-11
Mental, Behavioural and Neurodevelopmental Disorders. Consortium Psychiatricum, 2(2), 7-15. https://doi.org/10.17816/CP67
Sharan, P., & Keeley, J. (2018).
Cultural Perspectives Related to
International Classification of Diseases-11.
Indian
Journal of Social Psychiatry, 34(5),
1. https://doi.org/10.4103/IJSP.IJSP_45_18
Shields, M., Dimov, S.,
Kavanagh, A., Milner,
A., Spittal, M. J., & King, T. L. (2021). How do Employment Conditions and Psychosocial Workplace
Exposures Impact the Mental Health of Young Workers? A Systematic Review.
Social Psychiatry and Psychiatric Epidemiology, 56(7),
1147-1160. https://doi.org/10.1007/s00127-021-02077-x
Smirnova, M., &
Parks, A. C. (2018). Positive Psychology Interventions: Clinical
Applications. In D. S. Dunn (Ed.),
Positive Psychology: Established and Emerging Issues.
(pp. 276-297). Routledge/Taylor & Francis Group.
Stein, D. J., Szatmari, P., Gaebel, W., Berk, M., Vieta, E., Maj, M., de Vries, Y. A., Roest, A. M., de Jonge, P., Maercker, A., Brewin, C. R., Pike, K. M., Grilo, C. M., Fineberg, N. ,
Briken, P., Cohen-Kettenis,
P. T., & Reed, G. M. (2020).
Mental, Behavioral and Neurodevelopmental Disorders in the ICD-11:
An International Perspective on Key Changes and Controversies. BMC Medicine, 18(1), 1-24. https://doi.org/10.1186/S12916-020-1495-2
Strik, W., Stegmayer, K., Walther, S., & Dierks, T. (2017). Systems Neuroscience
of Psychosis: Mapping Schizophrenia Symptoms onto Brain Systems. Neuropsychobiology, 75(3),
100-116. https://doi.org/ 10.1159/000485221
Taylor, S. (2022).
Pandemics and Clinical
Psychology. In G. J. G.
Asmundson (Ed.), Comprehensive Clinical Psychology (2nd ed., pp.
151-166). Elsevier. https://doi.org/10.1016/B978-0-12-818697-8.00164-3
The Lancet Child & Adolescent
Health. (2018). What does ICD-11 Mean
for Child Health Professionals? The Lancet Child and Adolescent Health, 2(8), 543. https://doi.org/10.1016/S2352-4642(18)30211-6
The Psychology Practice. (2021). Diagnosis with DSM: An Interview with Professor Greg Murray. [Video]. Youtube. https://www.youtube.com/watch?v=-KOUNeGGdJw
Tyrer, P., & Mulder, R. (2022). Treatment and Outcome of Personality
Disorder. In Personality Disorder: From Evidence to Understanding (pp. 69-97).
Cambridge University Press.
Ulfa, M., Azuma, M., & Steiner, A. (2022). Burnout Status of
Healthcare Workers in the World During the Peak Period of the COVID-19 Pandemic.
Frontiers in Psychology, 13, 952783.
https://doi.org/10.3389/fpsyg.2022.952783
Vujnovic, M., Manukhina, O., Reed, G., Theodorakis, P., & Fountoulakis,
K. (2021). ICD-11 Revision of Mental Disorders: The Global Standard for Health Data, Clinical Documentation, and Statistical Aggregation. Consortium
Psychiatricum, 2(2), 3-6. https://doi.org/10.17816/CP74
Warren, A. (2017). WHO Improves ICD-11 focus on Mental Health Care in Primary Care
Settings. https://www.hcplive.com/view/who-improves-icd11-focus-on-mental-health-care-in-primary-care-settings
WHO Collaborating Centre for the Family of International Classifications (FIC) in the Netherlands. (2019).
Preparing the Region of the
Americas for ICD-11. https://www.whofic.nl/preparing-region-of-americas- for-icd-11
World Health Organization. (2021). Mental Health and Forced Displacement. https://www.who.int/news-room/fact-sheets/detail/mental-health-and-forced-displacement
World Health Organization. (2022a). Addressing Mental Health Through Primary
Care and Community Engagement in the WHO South-East Asia Region. https://apps.who.int/iris/handle/10665/361248
World Health Organization. (2022b). ICD-11, the 11th Revision of the International Classification of Diseases. https://icd.who.int/browse11/l-m/es#/http%3A%2F%2Fid.who.int%2Ficd%2Fentity%2F941859884
World Health
Organization. (2022c). ICD-11 2022 Release. [News].
https://www.who.int/news/item/11-02-2022-icd-11-2022-release
World Health
Organization. (2022d). ICD-11 International Classification of Diseases for Mortality and Morbidity Statistics: Reference Guide. https://icdcdn.who.int/icd11referenceguide/en/html/index.html
World Health Organization. (2022e). Mental Disorders. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
World Health Organization. (2022f). Mental Health at Work. https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work
Yang, M., Tyrer, P., & Tyrer, H. (2022). The Recording of Personality Strengths: An Analysis of the Impact of Positive
Personality Features on the Long-Term
Outcome of Common Mental Disorders. Personality and Mental Health, 16(2), 120-129. https://doi.org/10.1002/PMH.1548
Youmans, K. G. (2022). Background & Overview of ICD-11 Before
Implementation in 2022. In Yes-Him Consulting. https://yes-himconsulting.com/icd-11-overview/
Received: August 26, 2022
Accepted:
May 5, 2023
Este es un artículo Open Access bajo la licencia Creative Common (Atribución-NoComercial-CompartirIgual
4.0)